Meet Rachel Blair: The first Recreation Therapist to join the Mental Health Department at Unity Health
By Jessica Cabral
Recreation and leisure can help patients socialize, get active and learn coping strategies that they can take with them once they leave the hospital.
This is why Rachel Blair was hired to work in the 7M mental health unit and the Psychiatric Intensive Care Unit (PICU) at St. Joseph’s Health Centre, becoming the first Recreation Therapist to join a mental health program at Unity Health. With her education and training, Rachel brings a holistic approach to leisure and recreation as a means to promote healing.
Here, she discusses the types of initiatives she is bringing to help encourage movement, mindfulness and social connection, even at a time when we must remain physically distant.
What is Recreation Therapy and what does a Recreation Therapist do?
Recreation Therapy uses recreation and leisure therapeutically in a hospital setting to support the recovery model. Recreation Therapists use assessment, program planning, implementation, evaluation and documentation to help patients identify specific goals that they want to work on, such as stress management. We use leisure and recreation as the vehicle to help patients achieve these goals and build their coping skills. We also use interventions to help patients recover, such as wellness talks, mindful movement and therapeutic art.
For example, for some people gardening may be their way to tolerate stress whereas for others it may be going for a walk. Recreation Therapists always try to add meaning to people’s lives and we believe that the way patients use their free time can provide them with positive emotions, fulfillment and an opportunity to develop skills.
What types of initiatives are you bringing to patients in 7M and the PICU at St. Joseph’s?
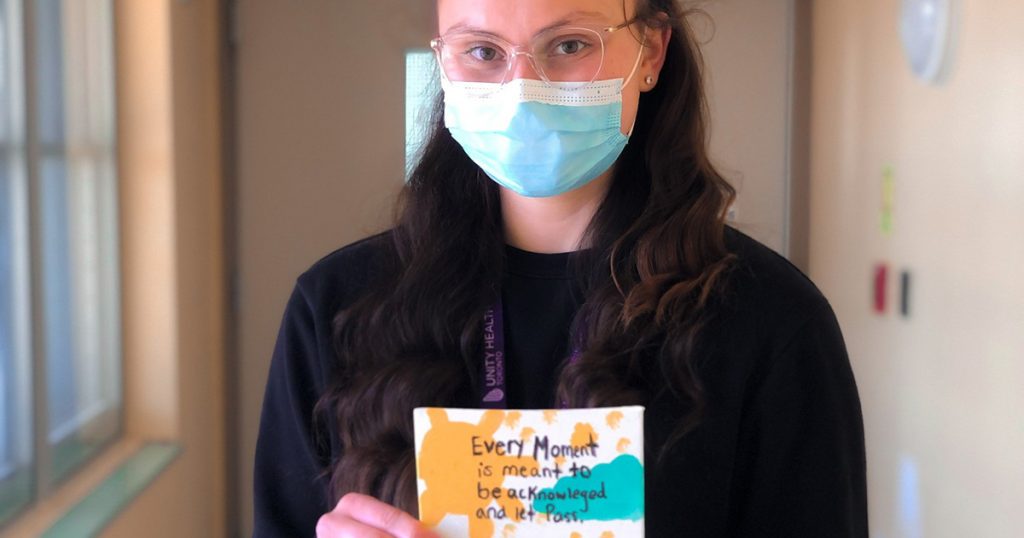
I like to introduce the patients to different types of kindness initiatives. In light of the pandemic, we started this activity called The Feel Better Letter. When patients arrive at the unit, they are placed in a seven to 10 day quarantine where they may be feeling lonely and isolated. Social connection is one of the most useful things in improving mental health and wellness, so through these Feel Better Letters we can bring a bit of joy and social connection to patients. All the patients who have finished their quarantine write letters to the patients currently in quarantine. Each letter describes how that patient had been in a similar situation, how they empathize with those in quarantine and how they understand the difficulty of being isolated during these hard times. Many of the patients are touched by the letters.
I’ve also been creating a program called Building Bliss. Through intentional activities like random acts of kindness and self-compassion, and gratitude, patients can use their free time to improve their happiness. The program will consist of different sessions like writing thank you letters, having a random kindness jar or even practicing savoring to teach patients to be more mindful while they eat.
Although an activity may appear as simply gardening or practicing yoga from the outside, each activity reinforces a skill for the patient. They leave and realize that they can use what they learned, like a breathing technique from yoga and apply it to when they’re having a panic attack.
How do you target your initiatives to meet the needs of the patients in 7M and the PICU?
It’s important to be adaptable and always listen to the patients to develop an understanding for what they might be interested in. For patients on 7M, they are further along in their recovery and they are suited for higher stimulation activities. This differs from the PICU where patients are earlier in their recovery journey and they need less stimulation and more of a stable environment.
Listening to the patients is crucial. There might be patients on the PICU who are interested in doing various types of gentle fitness, learning about different health teachings and exploring why exercise is important so I tailor my activities towards that. I also like to let members of the group teach their skills and share them with us as well. Sometimes patients will teach you new things. I once had a patient teach me Tai Chi and that was a cool experience.
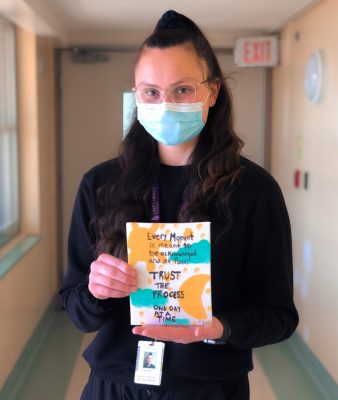
We like to empower the patients. Once, I noticed a space on a mural in the PICU that would benefit from the addition of an inspirational quote and instead of going ahead and adding it myself I involved the patients. One particular artistic patient loved the quote ‘This too shall pass’ so we took his idea and added it to the mural.
What types of recreation therapy activities can individuals do at home if they are struggling with their mental health?
One initiative that patients on the unit love and that I do as part of my bedtime routine is called Three Good Things, an activity adapted from the University of Berkeley. With this initiative, participants are asked to identify three specific good things that happened to them throughout the day and reflect on them. For example, someone could say ‘I had oat milk in my coffee today for the first time and that was a different experience’ or ‘I had a really nice interaction with another patient today.’ You can either write it down, say it aloud or just think of it in your head but it can help you to cultivate positive emotions and feelings of gratitude.
Another practice I would recommend is mindfulness and meditation, even for just 10 minutes a day. I like to teach and encourage that there is no right way to do it. Just sitting in the silence and focusing one the breath can be extremely impactful and healing.
I like to dance in my free time, some people love horticulture and buying new plants. It’s all about finding things that spark joy for you.
Above all, especially now during this COVID-19 pandemic, we need to find ways to connect socially. Find time to schedule a virtual coffee chat with a friend in British Columbia or somewhere else in the world. Make sure you maintain social connection.
What do you wish people knew about COVID-19, recreation therapy and mental health?
Now more than ever, recreation therapy in general and paying attention to how you spend your free time is essential for both patients and for ourselves. There is science, literature and evidence to back up the fact that the way you spend your time affects the way you feel. Focusing on what brings you joy can provide significant benefits for all of us. The best part of the job is that it’s so different for everyone I interact with. Some patients may enjoy juggling, or dancing, or some may like karate, while others may want to learn how to be more mindful to manage with their stress. There is a way to bridge all of those things together that will assist a patient with their recovery journey and build the skills they need to cope.
COVID-19 also highlights the importance of social connection. In the context of mental health, when patients come in they may have already been isolated in their houses or in the group homes that they live in. We have a psychiatrist here that says ‘social connection is nourishment for the soul’ and I really love that. One goal of my work is to connect people socially, even if that’s just one-to-one right now during the pandemic.
Is there anything else you’d like to add?
When working with the mental health population, it’s important to be an authentic practitioner. Through your actions, you can help a patient so much along their recovery journey. I always try to value and validate the ideas and thoughts that patients share. The patients on 7M and PICU as well as the staff are all extremely important parts of the patients’ recovery journey. We create a community here and I’m extremely grateful to be a part of it.
