BARLO MS Centre at St. Michael’s Hospital provides tailored care for patients with Multiple Sclerosis
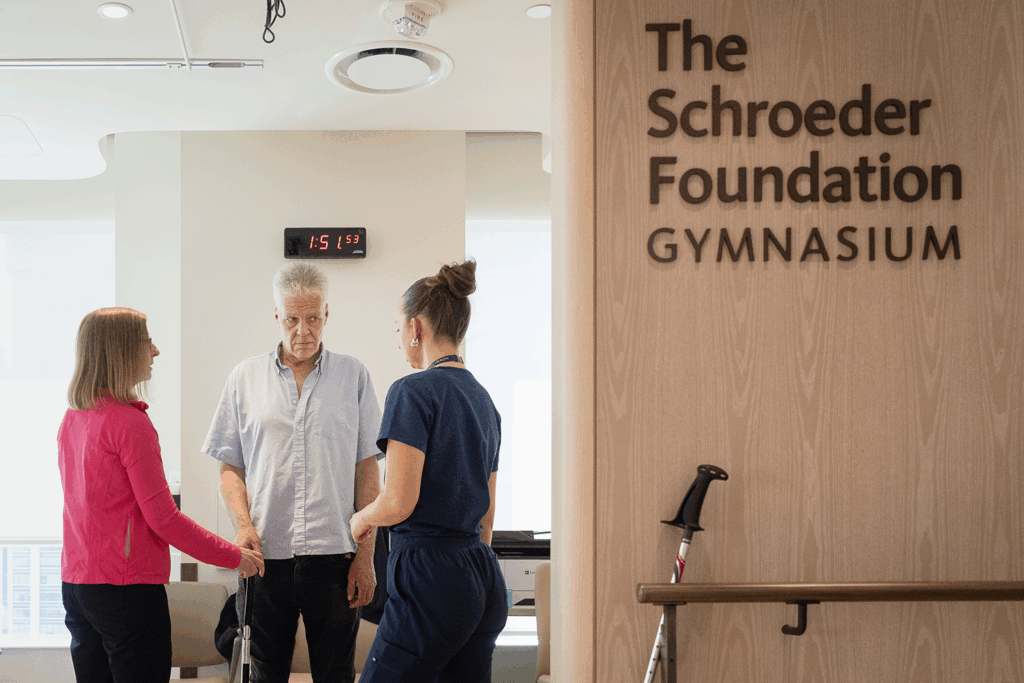
From left to right: Ellen Newbold, physiotherapist, Ian Lowe, BARLO MS Centre patient, and Sonia Gavrilova, physiotherapy student at the University of Toronto.
Ian Lowe was at work when he experienced a sudden shock through his neck, causing him to crash the machinery he was operating. He saw several doctors, who speculated that he might have tennis elbow or transverse myelitis – a neurological condition characterized by inflammation of the spinal cord. Two years later, at St. Michael’s Hospital, testing revealed a different diagnosis: multiple sclerosis (MS).
Lowe’s type of MS is progressive, which means that his neurological function worsens gradually or continuously, without periods of remission. Today, he struggles with his balance, hand function and pain in his neck. He also experiences stiff legs when he wakes up in the morning.
“Sometimes I get out of bed and I stumble,” he says. “Other times I find myself off balance, especially if I’m looking down and take a step backwards. I used to be able to hold a coffee in one hand and talk to someone, but I can’t do that anymore with my hand function.”
Enjoying this story? Sign up for the Unity Health Toronto newsletter, a monthly update on the latest news, stories, patient voices and research emailed directly to subscribers.
MS is episodic, meaning that the severity, type and duration of symptoms can vary from person to person. For many patients, like Lowe, both physiotherapy and occupational therapy play a crucial role in managing MS symptoms and improving overall wellbeing.
At the BARLO MS Centre at St. Michael’s – one of the largest of its kind in North America and one of only seven adult centres in Ontario – a team of occupational therapists and a physiotherapist offer unique, patient focused and evidence-based programming for patients who would benefit from support and education to maintain their independence or manage physical function.
Occupational therapists Marta Pogacar, Kelly Hennessy and Robin Lui, and physiotherapist Ellen Newbold, provide joint consultations, education, equipment trials, recommendations and community resources to BARLO MS Centre patients. Their work is filling a much needed gap in MS care and treatment in Canada.
“There are limited guidelines for occupational therapy and physiotherapy in terms of recommendations and treatments for people living with MS,” says Pogacar. “We’re in the process of conducting an environmental scan, and our findings have informed – and will continue to inform – new programming and referral pathways for BARLO patients.”
Health disciplines team provides joint consultation, resources and patient education
On a sunny spring afternoon, Hennessy and Newbold, accompanied by physiotherapy student Sonia Gavrilova, sit down with Lowe in the BARLO MS Centre gym. Lowe is here for a one-time assessment, after which the team can provide education, referrals to occupational therapists or physiotherapists in the community, strategies for self-management, alternatives to daily activities or other resources.
These one-time sessions allow the team to see as many BARLO MS Centre patients as possible.

“We have over 10,000 patients in the centre and while we’d love to provide ongoing support and therapy to all of them, we simply don’t have the time or resources,” says Hennessy. “This model allows us to see referrals at least once, and help them with a care plan or supports to move forward.”
At the start of Lowe’s session, the team asks if anything has changed since his initial telephone consultation in mid-April. Lowe says that he continues to struggle with hand function and neck pain, but he’s also having difficulty steadying himself when he gets out of bed in the morning.
“Do you notice if it worsens after activities or when you’re tired?” asks Newbold.
“I function at about 80 per cent energy always,” he says. “I might have sore legs the day after exercising or doing more activity but my fatigue and MS symptoms won’t be any worse than my baseline.”
Hennessy acknowledges that sometimes, a person may have sore legs but not experience changes in fatigue. She points to the concept of three batteries, in which everyone has a physical, cognitive and mood energy battery. If any one of these batteries gets depleted, you need to charge it, she says.
“Think of a phone. If it dies, it takes longer to charge,” she says. “Instead, you want to charge your phone periodically before that happens. This might look like sitting down between tasks. By shifting between the three energy batteries, you can avoid depleting one fully.”
Lowe says that physical energy is his biggest struggle, pointing to guitar playing as an example.
“I’m a musician and I can’t hold a guitar pick anymore,” he says. “I’ve had to adjust to finger picking.”
“That’s great if finger picking works for you,” says Hennessy. “It’s all about problem solving. We need to find different ways to keep doing the things we enjoy, even if that means some trial and error.”

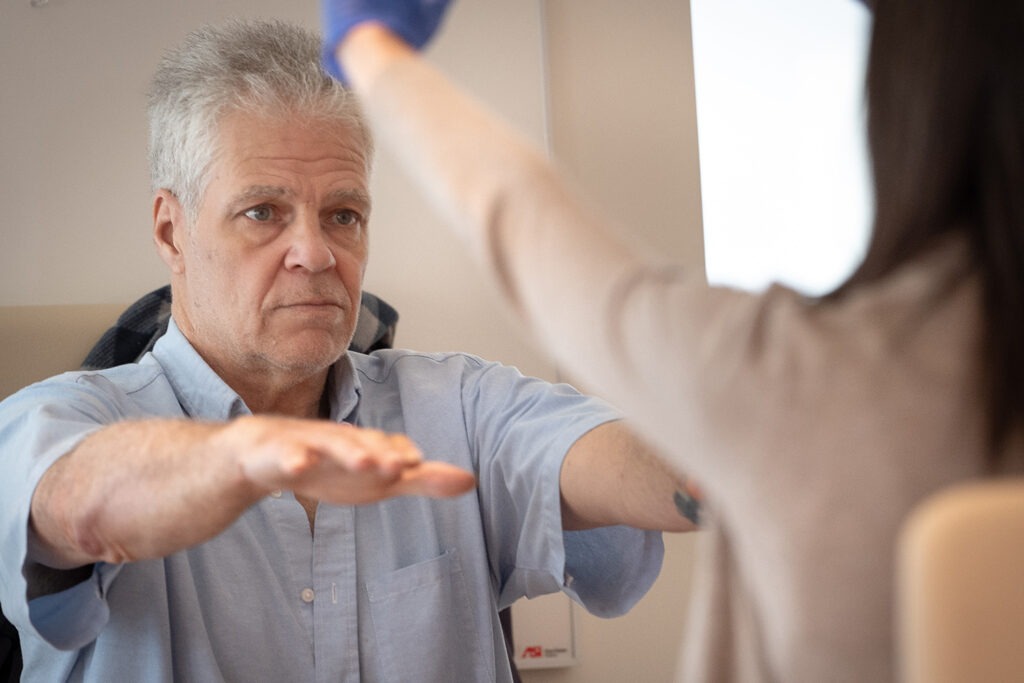
After some questions about Lowe’s day-to-day, Gavrilova assesses his lower body strength and movement. When she’s done, Newbold pulls her aside to review the assessment and discuss some tip sheets and exercises.
In the meantime, Hennessy assesses Lowe’s arms and coordination, then the team reconvenes to assess his walking, his ability to go up and down stairs and his balance. Newbold suggests that Lowe might want to consider a cane or walking sticks for additional balance support. Lowe says he’ll consider it.
Though Lowe doesn’t need it, the BARLO MS Centre features an Activities of Daily Living lab, where patients can learn how to modify their homes. Before Lowe’s appointment today, the team arranged for a community-based occupational therapist to assess his movements around the house.
“We look for as many ways as possible to support each patient, noting that everyone requires something different,” says Hennessy. “In Ian’s case, we wanted to make sure that he was getting the proper aids at home to improve his functioning and independence, and prevent falls or stumbles.”

At the end of Lowe’s session, the team sits down to discuss next steps. They give Lowe a series of activities, exercise-focused handouts for people with MS and falls prevention strategies. They suggest that he track his fatigue to see when he struggles the most, and remind him to take frequent breaks.
They also encourage him to use deep breathing or mindfulness when he feels stressed or overwhelmed, and to keep using his right hand for day-to-day activities.
“You’ve done a really great job finding strategies that pull you out of your stress and address some of the challenges you’re encountering with your hand function,” says Gavrilova. “These new strategies should help you address some of your ongoing challenges, like with your balance or leg stiffness.”
Lowe says he thinks they will.
“They’ve given me lots of valuable resources,” he says. “I’ll give everything a shot, to see what’s helpful for me. If something’s beneficial, I know I can stick with it.”
First-in-Canada program to address cognitive symptoms in patients with MS
Down the hall, Pogacar is beginning two virtual cognitive therapy sessions with BARLO MS Centre patients Sandra and David.
Many people with MS experience cognitive symptoms, such as difficulty focusing, making decisions or remembering things. These symptoms can affect a person’s independence and hinder their ability to complete simple tasks.
Pogacar is part of a team, led by Dr. Anthony Feinstein, a neuropsychiatrist at Sunnybrook Health Sciences Centre, that launched a research study in 2024 to understand whether people with MS could benefit from a computerized cognitive training program called RehaCom. Though not designed specifically for patients with MS, RehaCom contains several modules that help patients with specific aspects of attention, concentration, memory, perception and activities of daily living.

“RehaCom uses repetitive practice and gradual progression to target an impaired cognitive domain,” says Pogacar. “As occupational therapists, part of our role is to help patients find ways to cope with their deficits. We’re finding benefit in coaching patients to complement remediatory approaches – those that focus on restoring skills – with compensatory approaches – those that focus on working around limitations using alternative methods – to help generalize and optimize cognitve performance in their day-to-day.”
The results of the nine month study showed that RehaCom was most effective for certain people with MS. Based on these learnings, the study transitioned last month to a five-week online program, with one-on-one therapist support. The program is offered virtually, though patients have the option to complete the program in-person, if they prefer.
Sandra and David are two of 18 patients enrolled in the program’s first cohort. Each week, the participants complete two 40-minute sessions, each consisting of two modules. Today, Sandra and David are completing one module on vacation planning and another on grocery shopping. Both modules focus on executive functioning, with an emphasis on retention.
“What are some strategies that we can work on while planning a vacation?” Pogacar asks both patients before they get started.
“I need to be cognizant of the time,” says Sandra, who’s been having difficulty completing tasks, remembering information and keeping track of time.
David, who’s noticed changes in his processing time, says that he’s going to take time after reading the instructions to think about his plan before responding.
“Remember, you can always take breaks if you need to reset,” says Pogacar. “It’s better to take a break before we start to feel tired, to help our memory and physical symptoms. When our mind and body get pulled into a task, it becomes easier to forget things.”
Pogacar joined the BARLO MS Centre three years ago. She’s always had an interest in neuropathy but her connection to MS is personal.

“I have friends and family members who have been touched by MS, so I feel empowered to work in this space,” she says. “When I saw that there was an opportunity here, I thought, there’s no way, this is too good to be true. But they reached out and I was thrilled to accept.”
In her three years at the BARLO MS Centre, Pogacar has helped shape the clinic’s occupational therapy programming, filling gaps in community outpatient rehabilitation services.
“I spent a lot of time reflecting on how we, as the BARLO MS Centre, can continue to provide world-class care,” she says. “Together with the team, we reviewed our supports, our patient needs, our areas to grow, and how we can offer fair and equitable services to our patients. The goal isn’t to build just to build, but to build to provide the unique care that our patients need. This involves multiple perspectives, including those of patient and family partners.”
The cognitive rehab program was designed to help patients manage expectations and recognize where they have control. For instance, a person with MS may struggle to stay focused while grocery shopping, but by tweaking how they help themselves remember things, they can adapt or manage frustration.
“The patient is always the expert,” she says. “I can help them break down their tasks but it’s the patient who usually says hey, maybe I can do it this way. It’s so fun for me to see that creativity and the potential for patients to apply the strategies to other areas.”
Checking back in with Sandra and David, both patients say they took breaks to reset during the first module. David said he felt a bit frustrated towards the end.
“I had all this travel time but when I added in the taxi, that time went away,” he says. “Then, what I thought was the most direct route between destinations ended up taking longer.”

Pogacar acknowledges his frustration and suggests strategies to help him take in more information, establish plans and make decisions.
“When we have set timing and specific decisions we want to make, we can start with those,” she says. “If items are of equal priority, or there’s information we’re lacking, we have to triage them.”
Sandra and David each have one session remaining, then they’ll complete an assessment to see if their cognitive function has improved since they started the program. Other follow-up offerings and exit plans are in discussion as the program keeps growing.
“We’ll be able to see participants’ progression within RehaCom and from their pre and post-program assessments, but we’d like to do some more formal reassessments,” says Pogacar. “This is a unique program, so collecting more data can help us comment on effectiveness and feasibility in the long run.”
How collaborations are powering program development
St. Michael’s is a teaching hospital, and the BARLO MS Centre is no exception. Many of the centre’s programs and services rely on contributions from medical and health disciplines students at the University of Toronto. The centre also collaborates with care providers across the country, exchanging learnings and best practices for occupational and physical therapy.
“There isn’t much research guiding occupational therapists in the MS space, so we try to pull together and help each other,” says Pogacar. “The students are also a great resource; we learn a lot from them and they help us run a really busy clinic.”
Finishing up her last year of studies, Gavrilova says that her experience in the BARLO MS Centre has been invaluable.

“MS is very different for different people, so there isn’t a one-size-fits-all approach,” she says. “Getting to know each patient and find what works for them is rewarding and a great learning opportunity for me. I feel very safe here, which is a huge thing for a learner.”
Patient and family partners are also a key contributor to program development.
“Anytime we develop, we reach out to patients to understand what might be helpful and what their experience has been with that type of treatment previously,” says Pogacar. “These consultations invite patients and caregivers to share their experiences and feedback, to help us better understand the needs of our patients.”
In the coming weeks, the team is starting some new work to explore the feasibility of fatigue management programs. They’re also completing a study to better understand which patients are receiving referrals for physiotherapy and occupational therapy at the BARLO MS Centre.
“We want to make sure that the patients who need referrals are receiving them,” says Hennessy. “This means understanding the gaps and profiles of people who get referrals, such as certain symptoms or patient populations, and the ones who are being missed. This will help us inform future programming.”
The team has big plans, but if you ask their patients, they’re just grateful for the care they’ve received so far.
“The team has been great and the clinic’s fantastic,” says Lowe. “I just love this hospital. I was born here, so life seems to have gone full circle. It’s really nice.”
By Anna Wassermann
Photos by Kevin Van Paassen
