‘We would have never thought people would be living into their 80s’
What two HIV experts want you to know on World AIDS Day
For more than two decades, St. Michael’s Hospital has led the way in HIV care and is now home to Ontario’s largest HIV program in Ontario, serving 1,700 patients.
It is also where you’ll find two dynamic healthcare leaders who have been here since the beginning. Dr. Gordon Arbess launched his career as a family doctor drawn to helping patients experiencing this deadly disease. Back then, he was also referring patients to Dr. Sean Rourke, a young neuropsychologist and scientist trying to understand and improve promising new treatments. “We bombarded Sean in those early days!” Dr. Arbess laughs.
Today, Dr. Arbess is the Clinical Director of the HIV/AIDS program with the St. Michael’s Academic Family Health Team. Dr. Sean Rourke is a Scientist with MAP Centre for Urban Health Solutions and the Director of REACH Nexus, a national research group working on how to address HIV, Hepatitis C and other sexually transmitted and blood-borne infections.
We spoke with Arbess and Rourke about their long histories serving people with HIV and AIDS, how far treatment has come — and what still needs to be done.
Tell me about yourself and why HIV/AIDS is an area you’ve focused your career on.
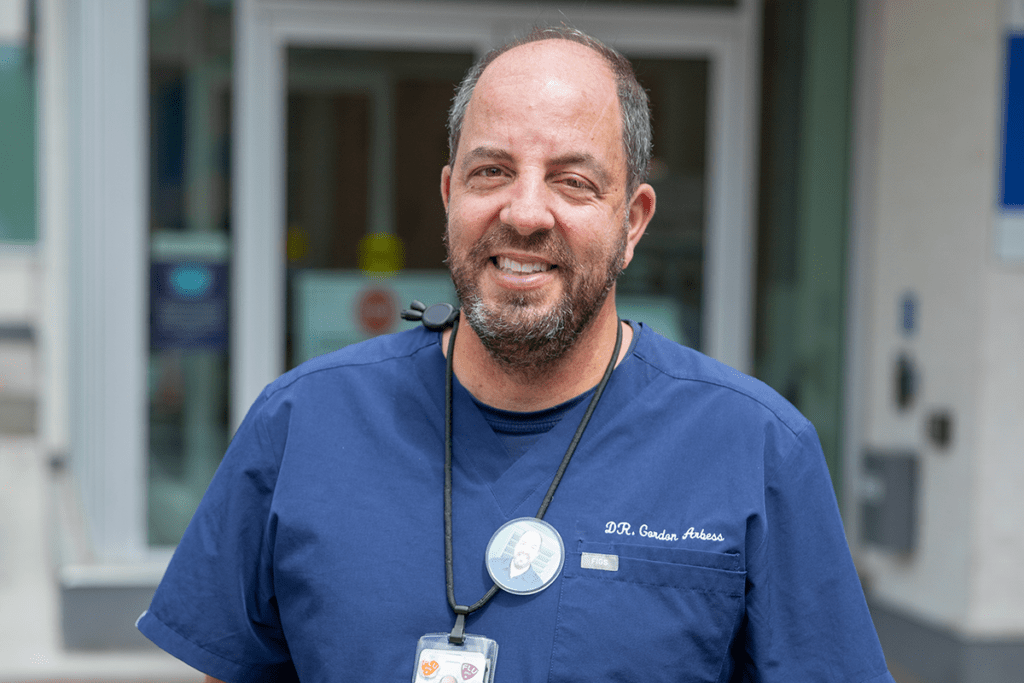
Arbess: I’m a primary care physician at St. Michael’s and I initially started my career at the Wellesley Hospital before it merged with St. Mike’s. I fell into this area because I did medical school at Queen’s University and while there, I met an individual who was single-handedly going into the community and penitentiaries to treat people living with HIV and Hepatitis C – I was really intrigued. When I moved to Toronto and did my residency with Wellesley Hospital, I was drawn to the work. When the hospital merged with St. Michael’s – a Catholic hospital – there were concerns among those of us doing this work about what that would mean. But it panned out beautifully and we’ve always felt well supported. I feel fortunate to be doing this type of work. It’s extremely rewarding work and it touches on all facets of humankind.
Rourke: I’m a neuropsychologist by training and a scientist, but I see myself more as a social entrepreneur now. I have a similar path to the start of my career as Gord – I started at the Wellesley-St. Michael’s Hospital. It was my first job and I’m still here! 1995 was a critical juncture in HIV because combination therapy was coming online. There was a lot of optimism that those therapies would ‘solve everything’. The concern at the time in my area of expertise was if the medications would eliminate dementia, and they have, but they haven’t eliminated this milder condition. So I was recruited to set up a clinical research program to explore the brain and cognitive health, and that’s how I started to work with Gord over 25 years ago.
St. Michael’s is a place with incredible, extraordinary people who are so committed, and like Gord said, to have the hospital behind the work we do on the clinical side, research, education – it makes our lives busy, we’re always over-extended – but it’s a real pleasure to be in a place where you get so much support. Today my work is about this: there are so many solutions, now it’s about getting them to people.
You have known and worked with each other for such a long time!
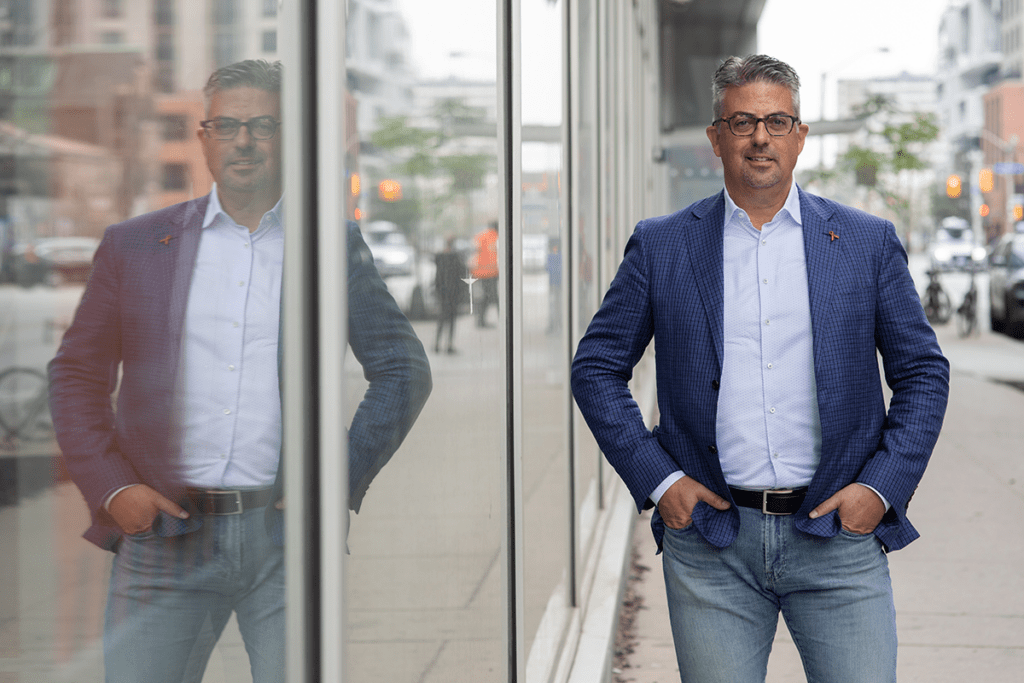
Rourke: I remember getting referrals from you, Gord, in early days. I was the new kid on the block in those first five years. I was one neuropsychologist with all these physicians and all their expertise and I remember thinking, ‘I’ve got to do a good job for this guy!’ Gord was always a leader in Ontario for new primary care doctors specializing in HIV.
Arbess: We bombarded Sean in those early days! He was the one guy who could do neuropsychological testing for these really complex patients and identify the problem and come up with solutions. Sean became the Executive Director of the Ontario HIV Treatment Network (OHTN), so we were involved in a different way because I coordinate the HIV fellowship to train residents to provide HIV care in Ontario, and the funding comes from the OHTN.
Can you reflect on how far have we come in preventing HIV and treating AIDS since you started your careers?
Rourke: The science of treatment is just huge. When we started and there were no combination therapies. People would take, 30, 40, 50 medications multiple times a day. Some had to be refrigerated, some not. Well if they have housing issues, how can we get them those meds if they don’t have a fridge? The complexity of where it started to now having injectables is just remarkable.
The science is giving options that work extremely well to keep people alive and help them live almost normal lifespans. People who have their virus suppressed can’t transmit, so it’s a huge public health benefit for people’s partners but also broadly. The science has been truly remarkable, not only in HIV, but think of all the treatments for cancer that really came from scientists working on HIV.
We have the science, we have the tools, now it’s all about getting to the 10 per cent of people we’re not reaching. How do you reach the people who are truly underserved and not getting the care they need?
Arbess: It is remarkable, I don’t think there’s any other field in medicine that’s changed as rapidly as HIV medicine. When we started around 1995/96, I remember going to the hospital and meeting patients with AIDS who needed follow-up with a family doctor and that’s how I built my practice. Some of those patients unfortunately passed away, but some of those very patients that I visited in ICU who were so sick are my patients today, and are generally doing very well.
At the same time, we have people who are unfortunately dealing with the problems of aging, comorbidities, the complexity of care, so they’re not only on medication to manage their HIV, but they’re on multiple other medications for cholesterol, diabetes, high blood pressure. These patients are more likely to develop these conditions a little earlier and are more likely to develop certain cancers. Because of the complexity medically, a lot of patients suffer from mental health conditions, addictions issues and they need a lot of support – this is where the team approach in their care comes into play. The majority of patients that we see, their HIV is very well controlled. It’s managing some of these other conditions that’s the challenge.
Our job now is to work with our patients to improve their quality of life, to have a normal lifespan, have relationships, have children – it’s a wonderful thing and people deserve that. When Sean and I first started, we would have never thought that people would be living into their 80s, having children, and continuing to work. So for the most part it’s a success story.
What do you want people to know on World AIDS Day?
Arbess: I feel like sometimes people don’t think HIV deserves a recognition day anymore, or that it’s not a real concern. I think it’s really important to understand globally the impact this disease has had and still has on people’s lives. There are millions of people living with HIV around the world, and many more who don’t know it. It behooves us to keep this condition on the radar, to talk about it, to identify those at risk of HIV and get them into care and provide them with the best possible care.
We should also understand that the care is very complex, people are aging with HIV and the other conditions I mentioned, that merit our ongoing care. I want people in the community to understand that this condition is still here, that we’re working as hard as we can to help people, and we’re going to need more help down the road. Not only are the patients getting older, but the practitioners and the providers are getting older. We need fresh providers to replace all those who are going to retire. There’s this constant pressure – who is going to look after these patients?
Rourke: The HIV/AIDS community, no matter where in the world, has always been a huge advocates for health access and equity. There are barriers to health care for people with HIV, but also for Black folks and Indigenous people. We want World AIDS Day to be every day – everyone should always have what they need. World AIDS Day is about highlighting success and recognizing the people that have come before us that have passed away. It’s also a day to recognize how we’re much more intentional now about inequities – people should be who they are and we are here to help them.
Arbess: That’s a really great point, I see World AIDS Day as a celebration, an acknowledgement of the great work and the advancement of the science. But it’s also a day to recognize the ongoing inequities – we know the burden of HIV populations will have more mental health issues, addictions issues. They’re more likely to be from Indigenous or racialized communities. The science is entrenched, we know what we’re doing in that regard, but we have a lot more work to do in terms of the inequities and trying to address those.
Rourke: Gord and I have been at this for a while. When you know what you know and you see what’s happening and know what’s available, you can’t help but wonder why we don’t just make sure treatment and care is there for everyone. Treatment works! When there’s people left behind, it’s clear that the entrenched systems are the barrier and that they don’t work for some people – and that’s not right, everybody should have the same access.
By Jennifer Stranges
This interview has been edited and condensed.
