Breastfeeding course at St. Michael’s aiding pandemic parents
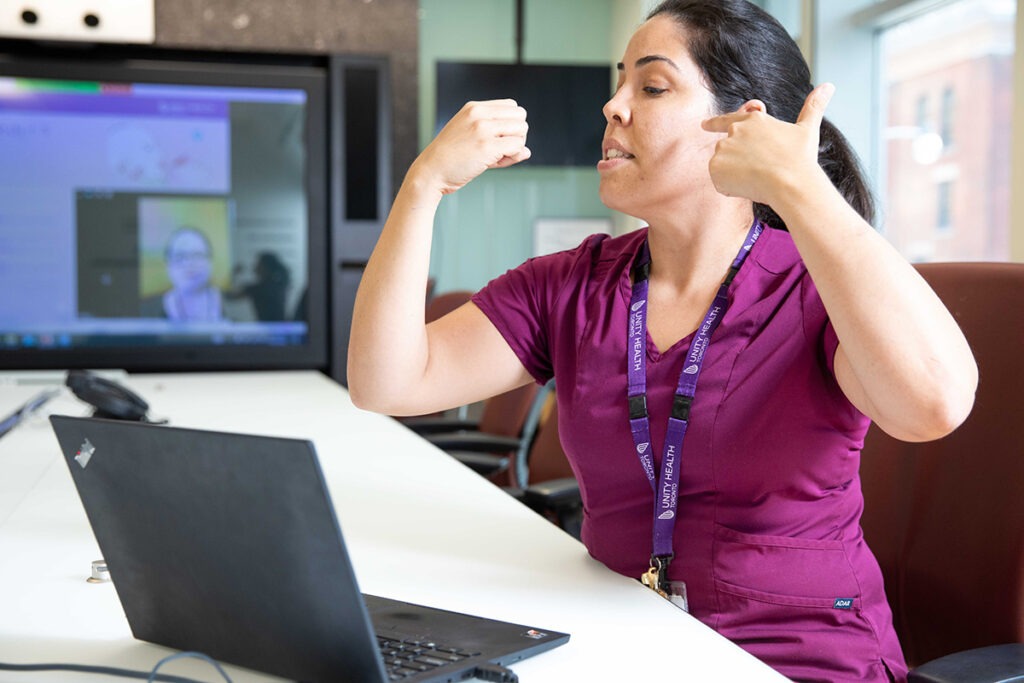
Camila Valente
One Tuesday a month, after a long shift at the St. Michael’s Hospital Family Birthing Unit, Camila Valente spends her evening teaching expecting families how to breastfeed.
The lactation consultant has been running the class over Zoom for six months, educating pregnant people about what to expect when they start feeding their infants. The course aims to familiarize parents with breastfeeding and empower them with the confidence to take care of their children.
“Providing preventative care and surrounding parents with information is the way to go when we’re trying to protect and increase the breastfeeding rates,” says Valente. Breastfeeding prevents many health complications for parents and children, she says.
Ninety-one per cent of parents in Ontario initiate breastfeeding after the birth of their children, but the rate of exclusive breastfeeding – infant feeding with breast milk only and no formula supplementation – drops drastically by six months.
At the beginning of the COVID-19 pandemic, Valente says she realized she needed to compensate for the lack of breastfeeding support available in the community.

Access to breastfeeding support was dire, especially as Toronto Public Health had to abruptly halt their in-home nursing support service and breastfeeding clinics at the start of the pandemic, recalls Amanda Hignell, clinical leader manager for the ambulatory women and children’s health clinics at St. Michael’s.
Families struggling with breastfeeding would have to turn to private lactation consultants – if they could afford them, she says.
“Having a baby at any time is very expensive, but we know the pandemic hit families really hard financially,” says Hignell. With an ongoing global formula shortage, the course helps families to save money on formula as well.
Valente says the pandemic widened pre-existing inequities in breastfeeding, due to a lack of services, support and information.
“What we are trying to do is just really bridge the gap,” she says.
“Camila is only one person when she’s seeing people in-person. In eight hours, she can only see that many families,” Hignell says. “Whereas she can see a whole bunch more in one class before birth to try to set them up for success.”
The two-hour class offers practical knowledge, such as identifying how and when to feed the baby, as well as positioning and assessing feeding quality. Valente also touches on the main struggles parents face, such as nipple pain, trouble latching and perceived low milk supply – one of the top reasons families start using formula.
“For some parents that are not familiar with breastfeeding initiation, when the baby is born and they’re not actually seeing the milk, or leaking, or spraying across the room, as I joke with my patients, they feel like they are failing,” Valente says.
Struggling with breastfeeding has a major impact on parental mental health due to feelings of guilt or shame, says Hignell.
“If we can help people by preventing some things that we know could potentially trigger post-partum depression, we’re setting up families that much more for success.”
Another advantage of the course is that it helps patients learn to problem solve on their own, especially as nursing shortages often prevent nurses from dedicating attention to non-acute emergencies, says Hignell. Nurses often provide support outside of business hours when lactation consultants are not present.
Valente says that so far, every class she has run has been fully booked. She is hoping she will be able to run the courses more frequently, and with larger class sizes.
The class has translated the knowledge in an efficient way, and families are being educated well virtually, says Valente.
“I’ve had the pleasure to work with some of the families here in the unit as well and the difference is crystal clear.”
She says she has noticed informed families are familiar with newborn behavior and with what to expect. Unless an emergency happens, she says, it’s all smooth sailing.
“It is really transformative when you see that family building their self-efficacy and reaching their own infant feeding goals,” she says. “I hope we can reach as many families as possible and in a larger scale and hopefully increase the breastfeeding initiation rates in Ontario.”
If you or someone you know is interested in taking this course, you can sign up here.
By: Talar Baboudjian Stockton
