‘A hospital without walls’: How Providence is supporting physical and social health care in vulnerable communities

By Christy Janssens
For many populations experiencing disadvantage in Toronto, accessing health care can be a challenge. Now more than ever, Providence Healthcare, Unity Health Toronto, is providing important support, bringing health care directly into the Oakridge community through an innovative model working directly with primary care physicians.
“I act as a client advocate in many ways,” said Sherry Qu, a Registered Nurse (RN) and Clinical Community Specialist, who was hired through Providence Healthcare to work with high-needs populations in Scarborough’s Oakridge neighbourhood.
Providence joined the Primary Care Interprofessional Care (IPC) team initiative in Oakridge alongside Michael Garron Hospital (MGH) and WoodGreen in 2017. Now, Providence, Michael Garron Hospital and the East Toronto Family Practice Network (EasT-FPN) work to deliver primary care and interdisciplinary services directly in high-needs areas of the community.
Many of the people Qu works with include those living with addiction, seniors, people with disabilities and refugees. Many live with a low income.
Qu, alongside Katherine Zgorzalewicz, another Clinical Community Specialist, and Dr. Drew Heyding, a community primary care physician and clinical lead, conducts regular clinics within Toronto Community Housing units in the Oakridge area, addressing issues like diabetes and high blood pressure.
“We’re fortunate that even before the pandemic happened, Providence made a commitment to this community,” says Dr. Heyding. “Providence has tried to be a ‘hospital without walls,’ in a sense, asking what they can do for this vulnerable population that lives right down the street.”
The team’s work also addresses social pressures and limitations that are known to impact a person’s overall health, such as helping create budget plans or get groceries when funds or mobility presents barriers, especially during COVID-19.
“It’s really about the social determinants of health,” said Dr. Heyding. “I can’t really take care of someone’s diabetes effectively if, for example, they have no stable way to get food or if they are in a lot of debt.”
Due to socioeconomic challenges, some people may not have a phone, television or internet access. Many speak a first language that is not English and some who do speak English have low literacy. These factors not only increase feelings of isolation at the best of times, but they can also make accessing both information and health care challenging during a pandemic.

Many tenants also live with mental illness and the increased stress of isolation and fewer options for in-person health care services can exacerbate those problems. Embedded health care professionals like Qu, Dr. Heyding and Zgorzalewicz are able to offer care to people in their own buildings, which can remove the stress that might be caused for someone already feeling overwhelmed by physically going to a hospital.
The team’s goal, Qu said, is to make things a little easier for all the residents in the community who need support. Health care, in this case, could look like helping someone renew their health card, create a plan to pay off a loan or navigate the bus system.
“We also want to decrease unnecessary emergency department visits in the area,” Qu said. “Because many people don’t have access to primary care, they will head to the ED. Our job is to assess the situation and point them to the correct services.”
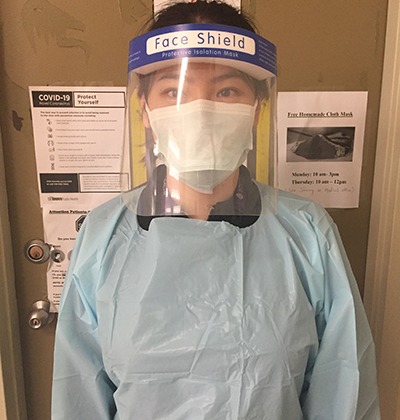
They also provide practical health education, offering accurate information about the nature of COVID-19, PPE, social distancing and more, from a trusted source.
“During the pandemic, we’ve been lucky to have Providence team members continue to be visible,” said Dr. Heyding. “They have already developed a footprint in these buildings. These are faces people trust, so they feel comfortable coming to us. We can catch things that might otherwise fall through the cracks.”
Even though it can be difficult, Qu said the work is fulfilling.
“This community collaboration has improved mental and physical health for so many people, she said. “My work is very meaningful because I see that we’re making changes in people’s lives.”
This initiative highlights the benefit of local organizations working closely to address the needs of complex populations. With the creation of the East Toronto Health Partners, the Ontario Health Team working together in East Toronto, Providence has continued to be involved in and contribute to these programs alongside Michael Garron Hospital and the EasT-FPN as anchor partners.
