First protocol developed to ensure the management of massive hemorrhage in Ontario is standardized across all hospitals
By Laura Bristow, Sunnybrook Health Sciences
A study published today in CMAJ Open outlines the design of Ontario’s first Massive Hemorrhage Protocol (MHP), a set of recommendations for hospitals that will enable rapid and coordinated delivery of blood products in a patient who is hemorrhaging.
Until now, there hasn’t been one standard protocol for all hospitals to follow when treating massively bleeding patients, said Dr. Jeannie Callum, lead author and transfusion medicine specialist at Sunnybrook Health Sciences Centre.
Co-lead author and transfusion medicine physician at St. Michael’s, Dr. Katerina Pavenski, said this new work will bring together the right care team to the right patient with the right resources.
To find out more about this work, we asked the research team more about their study and the impact of a protocol for Ontario.
Q. What is a massive hemorrhage?
A massive hemorrhage is large volume and rapid bleed that needs immediate stabilization through the transfusion of blood products and fast identification and treatment of the source of bleeding.
Q. How serious is a massive hemorrhage?
Massive bleeding is a leading preventable cause of death following trauma, childbirth, and surgery. There were 5.1 million deaths after traumatic injury worldwide in 2010, mostly affecting young people, accounting for nearly 10 per cent of all deaths. In the United States, it is estimated that up to 20 per cent of such deaths are the direct result of preventable hemorrhage.
Q. What is Ontario’s Massive Hemorrhage Protocol (MHP)?
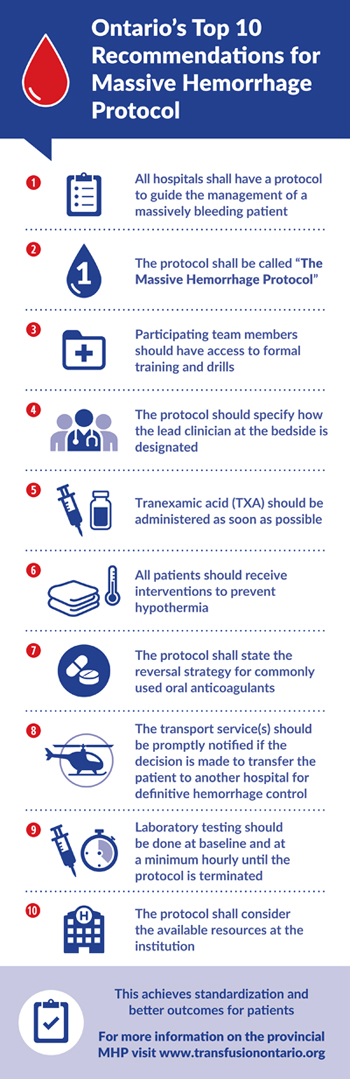
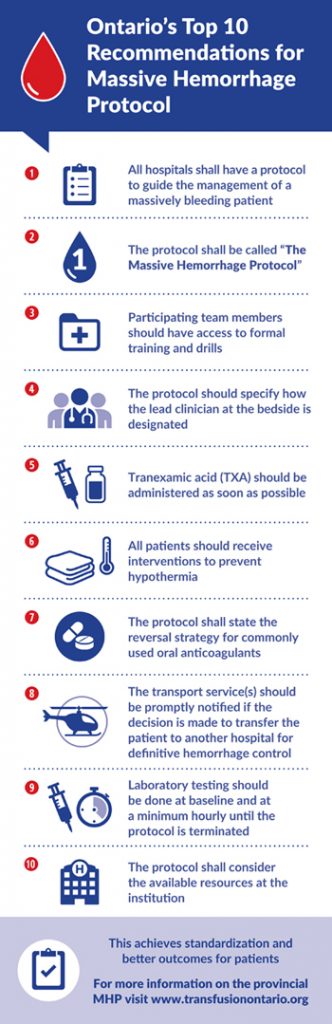
It is a clinical workflow for managing massive hemorrhage. Design of this workflow was based on the 42 recommendations and eight quality indicators. These in turn were developed through consensus of local experts including transfusion medicine specialists, surgeons, emergency physicians, nurses and laboratory technologists. MHP will standardize the approach to massive hemorrhage for all hospitals that supply blood in the province.
Q. How was the MHP developed
Not all MHP interventions are based on good quality studies. Therefore, we decided to use a Delphi method to reach consensus about what should be in our provincial plan. Delphi allows panelists to review and rate the proposed recommendations. The panelists were 36 experts from across Ontario and from diverse clinical backgrounds. Three rounds of review were held to reach agreement on the recommendations and indicators, which formed the basis of the MHP.
Q. Why don’t hospitals already have an MHP?
Developing a plan requires resources. Also, many smaller places encounter massive hemorrhage very rarely. Thus it is not surprising that many centres, especially smaller ones, have no formal policy to care for severely bleeding patients. This standardized approach will ensure hospitals all follow the same policy and care plan.
Q. Has an MHP ever been developed in another province or country?
A few other provinces have developed provincial MHPs, also a few countries have country-wide MHPs. What is unique about this endeavor is that it was developed by a rigorous consensus-building method and took into account special populations (ex. pediatrics, postpartum) and circumstances (ex. small hospital with limited blood product availability) rather than the one size fits all approach.
Q. How many patients will potentially be affected by the MHP on a yearly basis?
We know that there is, on average, one Massive Hemorrhage Protocol enacted every three days in hospitals like St. Michael’s and Sunnybrook. Given that this protocol will be the standard at all hospitals in Ontario it has the ability to reach and benefit hundreds of patients.
Q. What is the next step in the process for rolling-out the MHP to all Ontario hospitals?
The next phase of this work will be the creation of an actual template plan and MHP toolkit by the Ontario Regional Blood Coordinating Program which is funded by the Ministry of Health and Long-term Care Ontario. The toolkit will include specific recommendations for pediatric and obstetrical patients, and for hospitals with limited availability of blood components or means to achieve bleeding control. It will also provide suggestions on how to implement the plan, train staff and monitor quality indicators. This will give hospitals a sound launching off point to develop their own local policies and procedures.
About St. Michael’s Hospital
St. Michael’s Hospital provides compassionate care to all who enter its doors. The hospital also provides outstanding medical education to future health care professionals in more than 27 academic disciplines. Critical care and trauma, heart disease, neurosurgery, diabetes, cancer care, care of the homeless and global health are among the Hospital’s recognized areas of expertise. Through the Keenan Research Centre and the Li Ka Shing International Healthcare Education Centre, which make up the Li Ka Shing Knowledge Institute, research and education at St. Michael’s Hospital are recognized and make an impact around the world. Founded in 1892, the hospital is fully affiliated with the University of Toronto.
About Unity Health Toronto
Unity Health Toronto, comprised of Providence Healthcare, St. Joseph’s Health Centre and St. Michael’s Hospital, works to advance the health of everyone in our urban communities and beyond. Our health network serves patients, residents and clients across the full spectrum of care, spanning primary care, secondary community care, tertiary and quaternary care services to post-acute through rehabilitation, palliative care and long-term care, while investing in world-class research and education. For more information, visit www.unityhealth.to.