Trauma & Neurosurgery
Life-changing and life-saving care
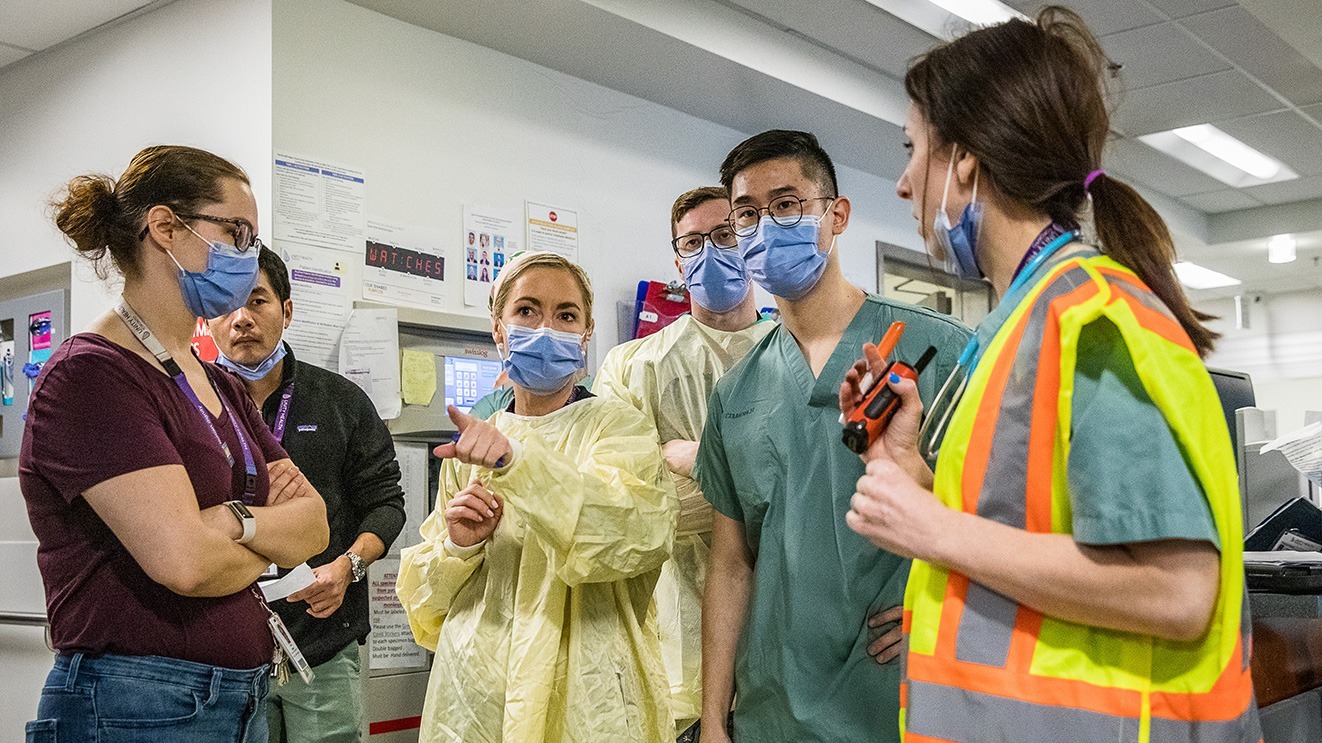
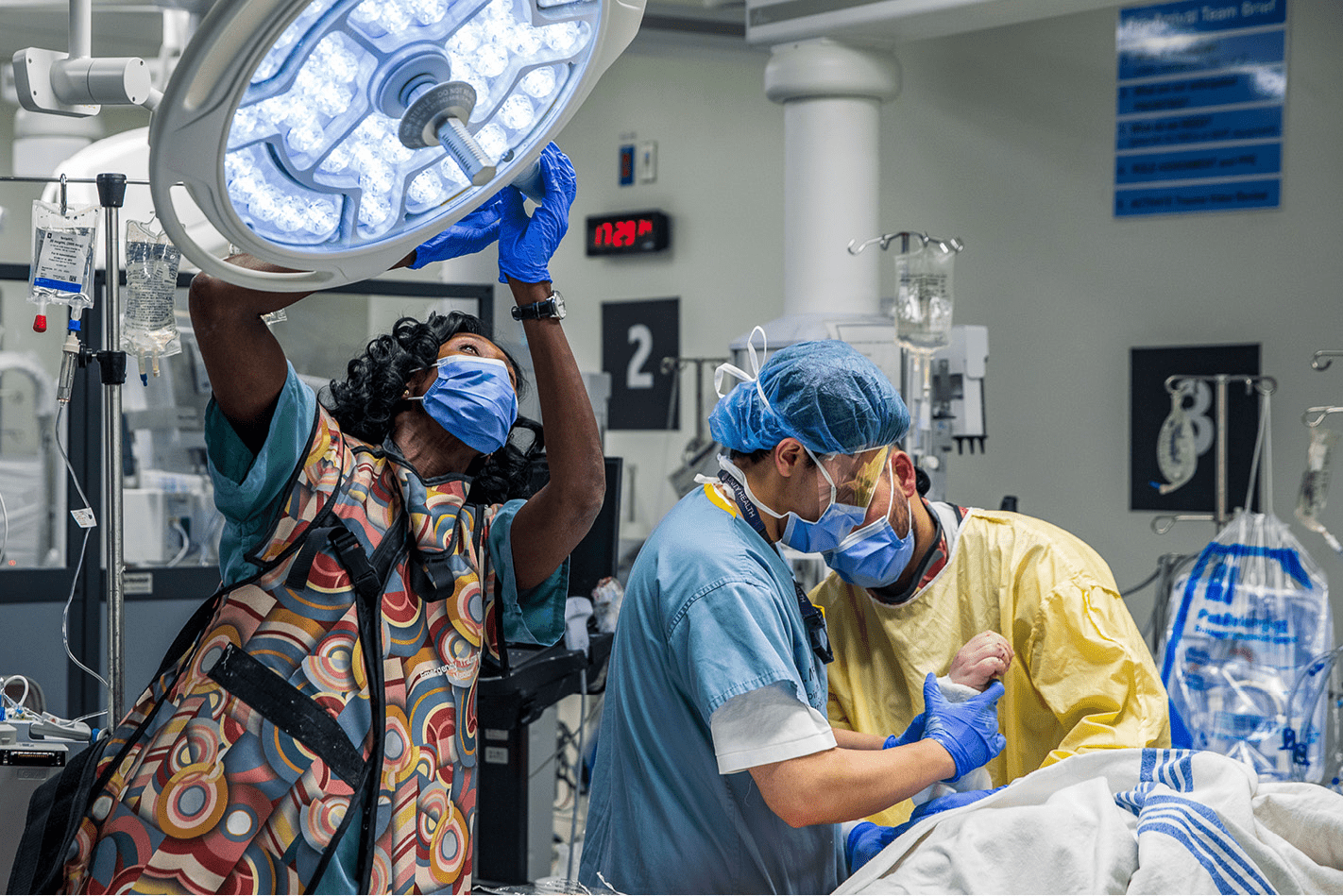
In trauma care, every second counts. St. Michael’s Hospital is one of only a few health centres outside of the United States verified as a Level 1 trauma centre by the American College of Surgeons, meaning people are rushed by air and ambulance from across Ontario to be cared for by best-in-class teams.
Unity Health Toronto’s neurosurgery program provides world-class care for the most complex case, using the latest technology to improve patient outcomes and groundbreaking research to advance care.
These elite teams are supported by radiology, transfusion medicine, emergency medicine, surgery, research, education, rehabilitation and more. Together, along with systems partners, Unity Health Toronto offers life-saving and live-changing care for people across Ontario and beyond.
Trauma & Neurosurgery at St. Michael's Hospital
St. Michael’s Hospital is an affiliate of the Neurosurgery Education and Outreach Network (NEON), which is a neurosurgery education support program reporting to the System Capabilities Working Group, a sub-group of the Provincial Neurosurgical Advisory Committee (PNAC), supporting system-wide improvements for Ontario’s neurosurgery services. NEON also works collaboratively with Critical Care Services Ontario (CCSO), which is the overseeing body responsible for the implementation of program initiatives of the Ontario Critical Care Strategy.
St. Michael’s Hospital works closely with community hospitals to optimize patient access and flow for neurosurgical patients to ensure patients are able to continue their care journey closer to home. Our advanced practitioners are dedicated to neurosurgery nursing program implementation and will support system-wide improvements through education and outreach across neurosurgery and non-neurosurgery centres (NEON Terms of Reference, revised April 17, 2018).
Contact information:
NEON is comprised of Neurosurgery Nurse Educators and Clinical Outreach Specialists/Advanced Practice Practitioners from each neurosurgery centre, supported by hospital administrators.
The representatives for NEON at St. Michael’s Hospital are:
Clinical Nurse Specialist: Neurosurgical Outreach, Trauma & Neurosurgery Program
Daniela Gaeta
Daniela.gaeta@unityhealth.to
Clinical Nurse Educator: Trauma & Neurosurgery Intensive Care Unit
Les Porter
Les.porter@unityhealth.to
Resources
- CCSO resources and education material
- Collar care
- Craniotomy: Post-operative complications
- E-learning module: Guidelines for basic adult neurological assessment
- Guidelines for adult spinal cord assessment
- Guidelines for basic adult neurological observation
- Intracranial pressure basics
- Neurosurgery consult referral guidelines
- Post-operative craniectomy care
- Subarachnoid hemorrhage: information and management
- Subdural hematoma: information and management
The Trauma and Neurosurgery Intensive Care Unit (TNICU) provides traumatic and neurosurgical care to patients from across the province.
9th Floor Donnelly Wing
416-864-5518
Clinical leader manager: Liz Butorac
Inpatient Unit
9th Floor Cardinal Carter Wing
416-864-5814
Clinical leader manager: Shannon Swift
Information to help you understand how your pituitary disorder will be diagnosed and treated at St. Michael’s Hospital.
ATLS
The Advanced Trauma Life Support (ATLS) course teaches a systematic, concise approach to the immediate management of the trauma patient. ATLS has been taught to more than 1 million doctors worldwide and provides a common language that can save lives in trauma situations. This 1.5 day Hybrid course includes 23 online modules that allow learners to study at their own pace prior to attending the hands-on course.
Course dates:
January 16-17, 2026
March 27-28, 2026 – 2-day Traditional ATLS Course (online modules replaced with in-person lectures)
June 19-20, 2026
July 24-25, 2026
August 14-15, 2026
September 18-19, 2026
October 16-17, 2026
November 13-14, 2026
Course fees:
Resident – $1400
IMG/PA/NPs – $1500
Physician – $1700
For more information or to register, please contact Anthie Dimoglou at Anthie.Dimoglou@unityhealth.to or 416-456-8216.
ATCN
The Advanced Trauma Care for Nurses (ATCN) course teaches well-established treatment methods and approaches trauma care in a systematic manner, presenting to the nurse a concise method of establishing assessment and management priorities in the care of the trauma patient. This 1.5 day Hybrid course is comprised of 23 online modules that learners may complete at their own pace. After completing these modules, learners will proceed to the course site to complete the hands-on skills portion of the course.
Course dates:
February 6-7, 2026
March 27-28, 2026 – 2-day Traditional ATCN Course (online modules replaced with in-person lectures)
October 2-3, 2026
Course fees:
RN – $650
Auditor – $250
For more information or to register, please contact Anthie Dimoglou at Anthie.Dimoglou@unityhealth.to or 416-456-8216.
ASSET
The Advanced Surgical Skills for Exposure in Trauma (ASSET) course is a one day cadaver-based course that presents key surgical exposures in five anatomic areas: neck, chest, abdomen and pelvis, and upper and lower extremities. Low student-to-faculty ratio allows for extensive faculty guidance during the hands-on portion of the course.
Course dates:
June 12, 2026
Course fees:
Surgical Resident/Fellow – $1500
Practicing Surgeon – $2000
For more information or to register, please contact Anthie Dimoglou at Anthie.Dimoglou@unityhealth.to or 416-456-8216.
ATOM
The Advanced Trauma Operative Management (ATOM) course increases surgical competence and confidence by teaching proper operative techniques for penetrating injuries. This one day advanced surgical course is intended for senior surgical residents, trauma fellows, military surgeons and general surgeons that would like to improve their skills in treating penetrating injuries.
Course dates:
May 27-28, 2026
Course fees:
Surgical Resident/Fellow – $1850
Practicing Surgeon – $2100
For more information or to register, please contact Anthie Dimoglou at Anthie.Dimoglou@unityhealth.to or 416-456-8216.
Preventable injury is the leading cause of death for Canadians ages one to 44. The impact of preventable injuries creates a ripple effect, impacting the patient, their families, friends and communities. The economic cost is also staggering: preventable injuries cost our healthcare system over $20 billion each year.
At St. Michael’s Hospital, our Injury Prevention Program is a vital part of our Trauma Program, focused on reducing the incidence and impact of preventable traumatic injuries. Through evidence-based education, community outreach, and advocacy, we aim to empower individuals and communities with the knowledge and tools needed to prioritize safety and injury prevention.
Injury prevention is not just an extension of trauma care—it’s a cornerstone of it. By proactively identifying risk factors and intervening early, we help reduce the burden on emergency services, shorten recovery times, and most importantly, save lives. At Unity Health Toronto, we believe that preventing injury is just as important as treating it, and we are committed to building a safer, healthier future for everyone we serve.
Upcoming Courses:
Stop The Bleed: November 5, 2025. 5 p.m. – 6:30 p.m.
Register via Eventbrite
Stop The Bleed: December 8, 2025: 1 p.m. – 2:30 p.m.
Register via Eventbrite
*Discount is available for staff/students/volunteers of Unity Health. Please contact us to access discount.
Trauma Injury Prevention Specialist: Emily Lanigan, Emily.lanigan@unityhealth.to.
Every patient who receives care in our trauma room at St. Michael’s Hospital is included in a study that records information about the care we provided. The study does not affect the care received, and it allows us to continue to improve the care we provide.
This study has the power to improve care for future trauma patients. Every patient who is included brings us one step closer to this goal.
Please click on the link below to learn more.
Clinics & Services
The Head Injury Clinic provides assessment, diagnosis and management of physical, cognitive and behavioural/psychological symptoms for patients who have sustained mild and moderate traumatic brain injury (mTBI). The clinic is run by a multidisciplinary team including physiatrists, neuropsychiatrist, RN clinical coordinator, social worker and cognitive speech-language pathologist.
Goals of the Head Injury Clinic:
- Early Assessment, diagnosis and comprehensive medical management (pharmacological and non-pharmacological) of TBI and related disability
- Coordination of community supports and rehab services
- Provide reintegration support for patients returning to work/school
- Collaborate with other providers across the system to best meet patient’s needs (OHIP and third party-funded services)
- Provide education related to mTBI to patients /family to guide them in their recovery
- Serving a unique patient population, this clinic is committed to providing excellence in care and effective treatments. Patients are referred directly from the Trauma Neurosurgery Department, Emergency Department and Family Practice at St. Michael’s.
The neurosurgery service at St. Michael’s is a busy inner city urban practice and one of 11 adult neurosurgical centres in Ontario. The Division of Neurosurgery distinguishes itself by providing neurosurgical care to patients with:
- Brain and spinal tumours
- Complex skull base lesions including pituitary tumours
- Spinal stenosis, spinal fractures and spinal cord injury
- Brain hemorrhages
- Neurovascular disease
The Neurovascular service provides highly specialized endovascular services for neurovascular disease including:
- Coiling/stenting of aneurysms
- Carotid artery stenting
- Vascular malformation management
RADIS Lab
Program Managers
 Nicole Cancelliere is the Neurovascular Research Program Manager at St. Michael’s Hospital and also works as a medical radiation technologist specialized in supporting neurointerventional & robotic-assisted procedures. She completed her collaborative undergraduate degree and X-ray technology diploma at Queen’s University and the Eastern Ontario School of X-ray Technology in 2013, and then went on to complete her Master’s degree in Neuroscience.
Nicole Cancelliere is the Neurovascular Research Program Manager at St. Michael’s Hospital and also works as a medical radiation technologist specialized in supporting neurointerventional & robotic-assisted procedures. She completed her collaborative undergraduate degree and X-ray technology diploma at Queen’s University and the Eastern Ontario School of X-ray Technology in 2013, and then went on to complete her Master’s degree in Neuroscience.
As a clinical research technologist, Nicole works with both the clinical and research teams, supporting innovative patient care in the field of brain hemodynamics and neurovascular disease. As co-lead of the RADIS lab, the collaborative research team uses advanced technologies, including Robotics, AI, Dynamic Flow, Imaging and Simulation, to develop
new approaches to improve diagnosis and treatment of neurovascular diseases. Nicole is certified as a specialized neurovascular robotic technologist and was a part of Dr. Pereira’s clinical team which performed the world’s first robotic neurovascular intervention in the world on November 1, 2019.
She is also very passionate about advancing minimally invasive neurosurgery and radiography training & education and has helped run several ischemic and hemorrhagic workshops globally using advanced simulators and 3D-printed vascular models. She is also actively involved with the Medical Radiation Sciences program at the University of Toronto and Michener Institute where she is involved in course development and interventional
radiology education. Nicole sits on the Canadian Association of Medical Radiation Technologists (CAMRT) Research Grant Committee that works to advance the field by providing financial support for worthy humanitarian, educational and scientific contributions through research by the profession. Nicole is committed to promoting a model of research integration with clinical specialty among future fellow technologists.
Eileen Liu is a certified Project Manager who is currently working as a Research Coordinator III for the Neurovascular Program at St. Michael’s Hospital. She obtained her Bachelor of Science (Honours) degree at Queen’s University and obtained her Master’s degree in Medical Science at the University of Toronto. Eileen is involved in the management and coordination of various clinical trials and projects involving neurovascular diseases including stroke, carotid artery stenosis, brain aneurysms, idiopathic intracranial hypertension, and more.
The STAND Clinic provides specialized care for patients with vertebral fragility and pathological fractures. Our multidisciplinary team of Neurosurgery, Anesthesiology, and Medical Imaging works together to support effective pain management and determine whether patients may benefit from procedures such as Kyphoplasty.
Eligibility
Patients may be considered for the clinic if they have:
- Back pain from a recent vertebral fracture
- Imaging demonstrating a recent thoracic or lumbar vertebral compression fracture
- A predisposition to fractures, such as:
- Confirmed cancer
- Osteoporosis
- 60 years old or over
Referral requirements
All referrals must include imaging confirming a recent thoracic or lumbar vertebral compression fracture. External referrals must include a recent MRI spine (<6 months) with STIR sequences.
View STAND ClinicInjury recovery and wellness
The Trauma Clinic at St. Michael’s is a Nurse Practitioner-led, post-injury assessment clinic for trauma patients who have received treatment in the emergency department or have been admitted to the hospital. The Trauma Clinic provides follow up care for patients who have sustained single and multi-system injuries related to motor vehicle collisions, gun violence, self-harm, falls or been injured in their place of work. Our team consists of nurse practitioners, nurses, social work and psychiatry.
Goals of the Trauma Clinic:
- Provide patients with comprehensive assessments to evaluate their physical, functional, cognitive and psychological recovery after injury
- Identify and provide early intervention to optimize post-trauma and injury outcomes
- Enhance collaboration with community teams to strengthen wrap around care
- Improve access to care and services after discharge that include: wound care, pain management, screening and referrals to specialty clinics and programs
Trauma stories

Last updated January 20, 2026