What makes research meaningful for patients? Including them from the beginning
How can health research best address the needs of the people it serves? For researchers at Unity Health, the answer is simple: involve patients, caregivers and community members from the start.
The Knowledge Translation (KT) Program at the Li Ka Shing Knowledge Institute, which works to turn discoveries into practice, has developed a program called Partners in Research, an online course to help patients and researchers collaborate on projects. Now, a published paper that looked at the program’s effectiveness – shows the course increased knowledge in patient-oriented research for patients and researchers.
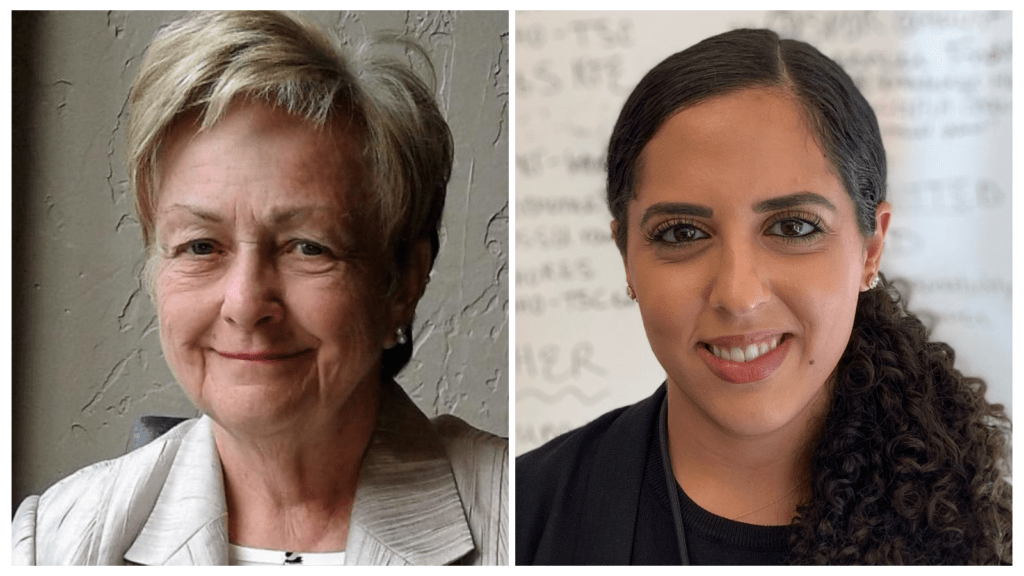
We spoke to two co-authors of the paper, Lorraine Bayliss, a Patient Family Partner, and Dr. Christine (Tina) Fahim, a scientist at the Li Ka Shing Knowledge Institute, to learn more about the program and how it’s bringing patient priorities into research.
Lorraine, as a patient partner, how did you get involved in research?
Lorraine: I was nominated by the Retired Teachers of Ontario to serve on the Ontario Drug Policy Research Network when I retired and I served for 15 years. I have lived with juvenile onset type 1 Diabetes for 50 years and hold a Masters of Education from the University of Toronto. Initially I was very involved in the training of all stakeholders – patients, health care providers, researchers, politicians – in patient-oriented research both in-person and online. I was engaged in delivering training modules with the Li Ka Shing Knowledge Institute, the University of Western Ontario Schulich School of Medicine and Dentistry, and Patient and Community Engaged Research initially out of Ottawa and now associated with McMaster and Western. One of the most important documents I generated was titled “The Art of Listening,” which shows the need to create a safe environment that is authentic where the patient feels comfortable telling their story.
If you do not get critical listening right and your judgment is not accurate then you stand to lose serious credibility. Narrative medicine, which is listening to the patient’s story, has been shown to improve health care outcomes for both the patient and health-care provider. As noted in a textbook on how to do primary care research, this partnership approach to research equitably involves individuals, patients, and communities and researchers in all aspects of the process and in which all partners contribute expertise and shared decision making and ownership.
Tina, as a researcher, why is it important for you to include patients and community members in the work you do?
Tina: At the Knowledge Translation Program we take very seriously this idea of integrated knowledge translation, which is the process of doing research both with and for the people which the project is going to impact. It’s not good enough to implement an evidence-based practice – it has to make sense for the people that it’s supposed to help and it’s hard to do that if you don’t have meaningful partnerships and deep rooted relationships with people, and if you’re not actually listening as a researcher.
This is something that we do quite routinely with almost every single one of our projects. We make sure that we have Patient and Family Partners at the table, and we’re hearing their voice and they are guiding our research.
What did you both learn from working together on this project?
Tina: We were able to build capacity in patient-oriented research. We had some metrics around knowledge and self-advocacy and those improved for both patients and the researchers who went through the course. There was also high satisfaction from both groups so to us that was encouraging.
There were also some lessons learned about things we could do better. The course was delivered online in 2017 and 2018. Now in this post-COVID world I think we’re much more used to doing everything online but at the time that was a limitation to people who didn’t have capacity to participate meaningfully online. It made us think about who are we reaching with these types of initiatives and what could we do to make it even more equitable, more inclusive, and how to sustain the work.
Lorraine: It was a very positive experience. I found that my voice matters and I participated fully in all aspects of the work. There was constant evaluation and looking at what can we do better. I want to see this continue because I truly feel that it’s a key to ensuring quality of life. For many people, especially people who live with a variety of chronic illnesses, or live in diverse communities, such as Indigenous populations, they need to be engaged in a way in which their experiences are truly valued. I would like to be involved in promoting this approach because it was one of the best experiences I have had.
There’s sometimes a disconnect between patient care and research and bringing the two together is an area that’s growing. What is the value of having patients at the table even when we’re doing very research-focused work that may not result in an immediate change for patients?
Lorraine: Lived experiences bring a great deal of insight. If people who do not have lived experience but have the knowledge to be able to research the challenges we share, and prevent complications, it can be a great savings on the health system and improve quality of life. That positive relationship between researcher and patient – the fact that you’re actively listening to the voice of people and making it a priority – is very valuable. Remember you never get a second chance to make a first impression.
Tina: InvolvingPatient and Family Partners at the very beginning can actually change our questions and outcomes. Often we go in with an idea of what the important outcome is, things like survival or death. Then you speak to Patient Partners and you learn that maybe survival isn’t the most important outcome. Maybe it’s quality of life, and we might not even be answering the right question if we don’t get that input in from the very beginning.
What can Unity Health and other peer institutions do to help promote patient and community engagement in Research?
Tina: It’s really about investing the time and the resources needed to do it properly. The last thing we want to do is be tokenistic or make somebody feel like we’re just there for an interview and we don’t actually do anything with their suggestions or their opinions. As a research team it’s also about building capacity to speak in plain language and to offer resources and capacity building throughout the spectrum of the project.
Lorraine, what is an example of a time you have been effectively engaged in research at Unity Health?
Lorraine: While serving on the Ontario Drug Policy Research Network, which is part of Unity Health, we were looking at biologics versus biosimilars in the field of insulin and diabetic care and cost savings. I talked about my early experiences with beef and pork insulin when the body saw it as a foreign substance and you just had to keep taking more. I felt that the biosimilars were less expensive, but still very effective. The CMAJ published our work. Li Ka Shing nominated me to be a patient partner with the University of Manitoba. Our research review has recently been published in the British Medical Journal. The team from Unity Health has opened many doors and paths in patient research that I never before anticipated.
Is there anything you’d like to add?
Tina: COVID has shown us more than ever why it’s important to have that patient voice and that public voice in research. We know based on COVID that efficacy of an intervention is not enough to ensure its implementation.
If we don’t understand the barriers and facilitators to why people do or choose not to engage in a certain intervention, or vaccine, or drug, then we have potentially a great intervention that that is not really going anywhere. The pandemic has opened our eyes to accessibility and equity challenges that we should seek to improve on going forward.
By Lorraine Bayliss
LISTENING IS AN ACTIVE PROCESS
- Focus and attention in a distracted free environment
- Interpreting the words for meaning and understanding
- Assessing the information with a view to next steps
- Seeking clarification
- Summarizing to ensure mutual understanding
- Using encouraging words that set the stage for “risk taking”
- Collaboratively establishing a plan of action
This interview has been edited and condensed.
Unity Health Toronto has a new resource guide for any researcher who wants to expand their knowledge of equitable patient and community engagement in the design and implementation of studies. Read the Guide here.
By: Ana Gajic
