Pituitary Innovation and Teaching
The Interdisciplinary Pituitary Disorders Centre of Excellence team at St. Michael’s Hospital welcomes you to our web page! This page is for people with pituitary disorders and their families. It is designed to provide you with general information about pituitary tumours, as well as with information to help you understand how your pituitary disorder will be diagnosed and treated at St. Michael’s Hospital.
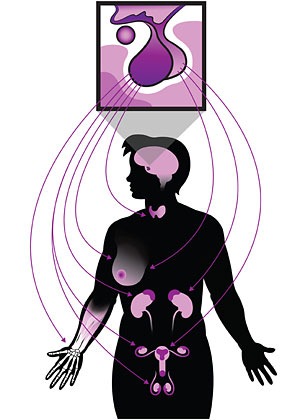
What is the pituitary gland?
The human body has many glands in it and these glands make hormones. Hormones help the body work. The pituitary gland is a small, pea-sized gland at the base of your brain. The pituitary gland is often called the “master” gland because it controls other glands in the body. The pituitary gland controls other glands including the thyroid gland, the adrenal glands, the ovaries, and the testes.
The hormones that the pituitary gland makes are involved in:
- how the body grows
- menstrual cycles
- how the body digests food (your metabolism)
- temperature and energy control
- making breast milk
- the balance of water in our bodies.
Pituitary tumours can affect these processes.
Patient information
Review the information below and/or our patient education brochure in:
More patient education booklets
Types of tumours and symptoms
A pituitary tumour (adenoma) occurs when the cells in the pituitary gland grow out of control and form a mass.
- Normal pituitary
- Small (micro) adenoma of the anterior pituitary.
- Large (macro) adenoma of the pituitary affecting eye nerve (optic chiasm).
- Large (macro) adenoma of the pituitary tumour growing down into sphenoid sinus.
Most pituitary tumours are not cancerous. The risk of the tumour spreading to other parts of the brain or your body is very low.
There are two types of pituitary tumours. One type is called a ‘functioning adenoma’, and the other is called a ‘non-functioning adenoma’.
Functioning adenomas may cause the pituitary gland to make too much of one of the pituitary hormones. If the tumour makes too much prolactin, growth hormone or ACTH, the patient will have changes in their body, depending on which hormone it is. Non-functioning adenomas do not make hormones. Both types of tumours can cause the pituitary gland to stop one or more of its normal hormone functions.
Both types of tumours can press on the nerves that help a person to see and so can cause problems with vision.
How common is it?
One out of every three people can have a pituitary tumour and never know it. This is because the tumour rarely grows large enough to cause any symptoms. Pituitary tumours usually grow very slowly. It may take years before people start to notice something is wrong.
How do I know if I have a pituitary tumour?
There are tests to see if you have a pituitary tumour. The tests measure hormone levels in your blood and urine. If your hormone levels are very high, this could mean that you have a pituitary tumour. Other tests are brain scans called MRIs or CT scans and vision tests to check eyesight.
Types of tumours and symptoms
There are two types of pituitary tumours. Both types can press on the nerves of your eyes and cause problems.
Types of functioning tumours (make too much pituitary hormone):
- Prolactin-producing tumours (Prolactinomas)
- Growth hormone-producing tumours (Acromegaly)
- ACTH-producing tumours (Cushing’s disease)
Non-functioning tumours:
- Non-functional pituitary adenoma
- Craniopharyngioma
The following are other common pituitary diseases:
- Rathke’s cleft cyst
- Pituitary apoplexy
- Craniopharyngioma
The symptoms that are caused by a pituitary tumour depend on:
- the size of the tumour
- how it affects the making of hormones in your body
- how the tumour affects your brain and eyes.

Abnormal secretion of breast milk (galactorrhea)
Prolactin-producing tumours make too much of a hormone called ”prolactin”. These tumours are called “prolactinomas.”
Women with a prolactinoma may:
- stop having their menstrual period
- produce some breast milk (a condition called “galactorrhea”)
- become infertile (unable to have babies)
Men with a prolactinoma may:
- get headaches
- have problems with sexual desire or function
- lose peripheral vision (off to the sides) and only see straight forward.
Medicine can reverse these effects. Prolactinomas respond to medicine and rarely need surgery.
Growth hormone-producing tumours make too much growth hormone. These tumours lead to a disease called ‘acromegaly’. Acromegaly affects adults, children and teens in different ways.
Adults:
Acromegaly in adults causes the hands, feet, forehead, nose, lips, tongue, and internal organs (like the heart) to get bigger.
In adults, acromegaly can lead to:
- high blood pressure
- high blood sugar
- heart disease
- snoring and breathing problems during sleep (known as sleep apnea)
- sweating
- skin tags (little growths on the skin)
- premature heart attacks
- growths of lining of the intestine
- nerve pressure in the wrist (carpal tunnel syndrome)
Surgery is the most common method for treating acromegaly. Medicine and/or radiation can also help to decrease the amount of growth hormone. If all parts of the tumour are removed with surgery, some of the effects of acromegaly will start to reverse.
- Enlarged hand and foot in a patient with acromegaly
- Acromegaly causes physical changes such as enlarged facial features and skin tags (litle growths on the skin)
Children and teens (before puberty)
In children and teens, who have not started puberty yet, making extra growth hormone causes “gigantism”. Gigantism makes children and teens very tall. The reason why acromegaly results in gigantism in children and teens only (and not adults) is because children’s bones are still growing. Surgery is often the common method for treating acromegaly and gigantism. Medicine and/or radiation can also help to decrease the amount of growth hormone. Even if all parts of the tumour are removed with surgery, those who have grown very tall will remain tall.
Non-functioning tumours are different from the functioning tumours described above. Non-functioning tumours do not make hormones. They are usually found during tests for headaches or loss of vision. These tumours tend to be larger than functioning tumours. They may continue to grow, press on the normal gland and cause the pituitary gland to stop making some or all hormones. This is called hypopituitarism.
Hypopituitarism can cause:
- low energy levels; tiredness
- dizziness
- nausea and loss of appetite
- feeling very cold
- constipation
- weight gain or loss
- slowness of thought
- loss of menstrual periods in women; loss of sexual function in men
The treatment for hypopituitarism is to give the patient back the hormones they are lacking.
Craniopharyngioma
A craniopharyngioma is a rare non-cancerous tumour that develops above or in the pituitary gland. This type of tumour can cause headaches, vision problems, hypopituitarism, memory loss and reduced growth. Having a craniopharyngioma can also make the patient very thirsty and want to urinate more (this is called “diabetes insipidus”). Treatment for a craniopharyngioma is to remove the tumour with surgery and sometimes with radiation.
- A Rathke’s cleft cyst is a pouch filled with fluid, and it sits inside or above the space where the pituitary gland is. If the pouch gets bigger, it can cause a loss of hormones, headaches or loss of vision. Surgery is usually the best way to take out the cyst and prevent further damage. You might need to have surgery if the cyst comes back.
- Pituitary apoplexy happens when any type of pituitary tumour gets suddenly bigger or bleeds. When a tumour gets bigger or bleeds, you may feel a lot of pressure in your head, have a sudden, severe headache, loss of vision or double vision. In rare cases, you may have altered consciousness and shock. It is important to go to the doctor right away if you feel this way if you have a pituitary tumour.
What kinds of health care providers will help me manage my pituitary tumour?
More than one kind of doctors will be involved in your care since a pituitary tumour can affect your hormones, vision, and brain. These doctors include:
Neurosurgeon – Brain surgeon
Endocrinologist – Hormone specialist
Radiation oncologist – Cancer specialist (uses radiation therapy to treat tumours)
Otolaryngologist – Ear Nose & Throat (ENT) surgeon
Ophthalmologist or Optometrist or neuro-ophthalmologist– Eye specialist
Psychiatrist – Mental health specialist
Anesthetist – Doctor who gives anesthetic and pain killers for the surgery
Family doctor – Provides long-term care and general medical care to all family members
All of the doctors will ask for a history of symptoms and do a physical exam. Some of the doctors will focus more on certain areas, such as the eyes for the ophthalmologist and the nose for the ENT surgeon.
A number of other professionals, such as nurses, social workers, physiotherapists, and pharmacists may help with care as well. Several sorts of nurses are involved in care, each within a special area and a different role: the pre-admission clinic prior to surgery; in the surgery preparation area, the operating room, the recovery room, and in the various hospital wards.
Blood tests
Blood tests are done to check hormone levels and other things like a person’s blood type, blood chemistry or blood counts. They are done before visits with the neurosurgeon and endocrinologist, before surgery, right after surgery, and for follow-up visits.
Before surgery:
- If possible, come to St. Michael’s Hospital’s blood lab for blood tests. Come between 7:30 a.m. and 9 a.m. since hormone levels vary at different times of the day. An appointment is not needed, but if you live too far away, you can do the blood tests at a location closer to where you live.
Blood tests will also be done during the pre-admission appointment, right after surgery and for follow-up visits with the doctor. These blood tests help doctors check hormone levels and how they might affect your body.
Since hormone levels vary over they day, for the best accuracy, the blood tests should be done at 8 a.m. If you are taking the hormone medicine Hydrocortisone (Cortef®), hydrocortisone, or prednisone, the blood tests should be done 24 hours after your last dose of medicine. This means, for instance, that if you are doing the blood test Monday morning, your last Hydrocortisone (Cortef®) pill should be Sunday morning, then you take the next pill right after you do the blood test. If you have questions about your blood tests, ask your doctor.
Vision tests
These tests are important to accurately measure vision and check the health of the nerves to the eyes.
Visual field test
Prior to coming to the appointment at St. Michael’s, ask your eye doctor, family or referring doctor to arrange for a “visual field test” to check your peripheral (side) vision. The test, requires concentration, does not hurt, and requires that a button be pressed every time a flash of light appears in a screen.
After you have a visual field test, your neuro-ophthalmologist will decide if you will need more eye testing. The following are two other tests they may arrange for you.
Optical Coherence Tomography (OCT)
This is an ultrasound test to measure the thickness of the nerve in the back of the eye (i.e. optic nerves). This test can tell if the nerves of the eyes have ever been damaged.
The OCT may not be covered by provincial health insurance. Please ask your ophthalmologist for more information about the cost of an HRT.
Visual Evoked Potential
A Visual Evoked Potential test will help your doctors know if the nerves of your eyes have been damaged by the tumour. This test involves flashing a light in your eyes while a machine measures the amount of time it takes for your brain to record the visual signal caused by the flash of light. If the brain takes a long time to record the visual signal, this tells your doctor that there is damage to the nerves of your eyes.
Preparing for a visit with the neuro-ophthalmologist:
- Arrange for someone to drive you home from the appointment. The eye drops used during the visit will make it hard to focus.
- Bring eyeglasses
- Bring sunglasses to wear home after the test
Imaging
Magnetic Resonance Imaging Scan (MRI)
This test gives doctors pictures of the pituitary gland and surrounding brain. The test is often done in 2 steps. First one set of pictures is made and then right after, a second set is taken after injection of a dye into the vein through an IV (intravenous) line. This test is done before and after surgery and during the follow-up for years after surgery.
Computed Tomography Scan (“CT” or “CAT scan”)
Computed tomography (CT) is a test that combines X-rays and computer scans. The pictures provide very detailed pictures of the bones in the nose and the bottom of the skull to help provide accurate guidance during surgery. This CT scan should be done at St. Michael’s.
Note: If the MRI was done at a hospital other than St. Michael’s, make sure to bring a copy of the MRI (loaded on to a CD-ROM or DVD) to the appointment with the neurosurgeon or endocrinologist.
Other tests
Hormones affect many internal organs and how your body functions. This means your doctors may need you to have tests to check your:
- heart (echocardiogram -ECG)
- intestines (colonoscopy)
- bones (bone mineral density for osteoporosis)
- prostate (for men only)
- sleep (sleep study).
Types of treatment
There are several types of treatment. These include:
Surgery is often the best treatment option for patients with a pituitary tumour who are healthy enough to have surgery and any of the following:
- whose tumour is putting pressure on or damaging the nerves of their eyes (optic nerves or chiasm)
- whose tumour is making too much hormone, such as growth hormone or ACTH
- whose prolactinoma is not responding to medicine
- whose tumour is growing
- whose diagnosis is not clear from other tests
- whose tumour has come back after surgery or is causing a leakage of brain fluid after surgery
Goals
The goals of surgery are to:
- diagnose the type of tumour
- reduce pressure on important structures like the nerves of the eyes
- remove as much of the tumour as possible (this reduces the chance of the tumour coming back)
- help reduce symptoms like headaches, visual loss, and high or low hormone levels
Types of surgery
There are two types of surgery for removing pituitary tumours: “transphenoidal” surgery or a “craniotomy”.
Transphenoidal surgery is done through the nose (see Figure 7). This method helps the surgeon access the base of the brain where pituitary tumours usually are.
A craniotomy is a type of surgery where the surgeon opens a window in the skull to access the tumour, instead of through the nose. This may be the best type of surgery if the tumour:
- is large
- is of a certain type
- goes off to the sides
- lies deeper in the brain
How does transphenoidal surgery work?
- A general anesthetic to put the patient asleep is required.
- During surgery, a small telescope with a tiny video camera at the end called an “endoscope” is guided through the nose and nostril passages to the tumour.
- The surgeon will remove small pieces of bone to expose the pituitary gland and the tumour.
- The surgeon will then remove the tumour. If the tumour is too large or if it is stuck to important structures in the brain, it may not be possible to remove the whole tumour.
- The bones are usually replaced with a tiny amount of biological glue and can be covered with a layer of the nasal cavity lining called mucosa.
- If there is a leakage of brain water called cerebrospinal fluid, some small pieces of fat or tissue that covers the thigh muscle will be taken from the side of the thigh or lower tummy to close the surgical area.
- The surgeon will check for any leaking from your nose. Occasionally, if there is a large amount of cerebrospinal fluid (also called CSF) leakage there is a risk of developing a serious infection called meningitis. If this fluid is leaking a lot during or after surgery from your nose, the surgeon may place a drain in the lower back. This drain will allow the CSF to drain out into a bag for a few days. Draining the cerebrospinal fluid will relieve the pressure in your nose and allow your incision to heal.
- Once the surgical area is sealed, two small plastic sheets are put in to the nose to prevent the growth of scar tissue. These sheets will be removed by the ENT surgeon two to three weeks after surgery.
- At the end of the surgery, the nostrils are packed with Vaseline gauze or a sponge to prevent nose bleeding.
- The surgery usually lasts a total of three to six hours but it depends on the tumour size, tumour extent, texture, and whether scar tissue exists.
What is the success rate?
The success rate of surgery for all kinds of tumours depends on the size and extent of the tumour, texture (firm or soft), and type of tumour. In most cases, if vision is impaired but still present before surgery, there is a good chance that the vision will be preserved and some chance of improvement, even if the tumour is large. If the tumour extends around the artery, tumour will usually remain after surgery. In the case of functioning tumours like Cushing’s disease, the success rate is better if the tumour is visible on MRI and localized. Tumours that are invading structures around the pituitary gland, are growing rapidly or are regrowing have a lower chance of success.
What are the risks?
At St. Michael’s Hospital, pituitary surgery is done often and is very safe. However, just as with any surgery, there are risks. Patients and families should ask questions and discuss the risks and benefits of surgery with their doctors before surgery. Some of the risks and the potential outcomes of these risks are listed below:
| Risks | Potential Outcomes |
|---|---|
| Damage to pituitary gland | Loss of hormone functions. This might require taking hormone replacement medicine(s) (for replacing one to six hormone(s) either temporarily or permanently. |
| Damage to blood vessels (i.e. carotid arteries) that are around the pituitary gland | Stroke, a lot of blood loss, or death |
| Damage to lining of the brain | Leakage of brain fluid and may cause an infection called meningitis |
| Vision problems due to damage to the nerves of the eyes | Partial or complete blindness in one or both eyes |
| Scar tissue formation or crusting in the nose | This can lead to nasal obstruction or bad smells because the nose is not being cleaned properly |
| Sinus infection | Loss of smell and/or taste, need for antibiotics and nasal rinsing |
After discharge from surgery
If you have had surgery: On average, patients stay in the hospital for two to four days after surgery. Once doctors are happy with your course in hospital, your will be discharged home. A family member should arrange to take you home before 11 a.m.
The nurses will teach you:
- how to rinse your nose with salt water on a daily basis,
- explain the follow-up plans and appointments
- provide a discharge summary for your family doctor
- go over “dos and don’t’s”
- the following appointments for after surgery should be made by the staff on the neurosurgical floor:
- one to twoweeks – you should see your family doctor
- two to three weeks – ENT – appointment with nose specialist
- three to four weeks – Endocrinologist appointment
- four weeks – Visual tests and ophthalmologist
- four to six weeks MRI
- six to eight weeks – neurosurgeon appointment
- Longer term – usually follow-up with your endocrinologist and neuro-ophthalmologist as determined at your last checkup
Radiation therapy uses high-energy X-rays to control the growth of tumours. Radiation therapy can either be used after surgery or in cases where surgery is not an option. Radiation can also be very useful if the whole tumour cannot be removed during surgery and continues to grow, or if a tumour recurs after surgery.
There are a few ways to get radiation therapy. Your doctor will discuss which option is best for you:
- Fractionated radiation
- Stereotactic radiosurgery – Single dose radiation therapy
Fractionated radiation
In fractionated radiation therapy, patients get a small amount of radiation five times a week for four to six weeks. Because a small fraction of the total dose is given each weekday, it is called “fractionated”. Each treatment may last for 15 to 20 minutes per day. The radiation can be given in a variety of ways. In intensity modulated radiation therapy, the radiation is given precisely to an area slightly bigger than the tumour. This makes sure that the whole tumour gets radiation. The treatment is carefully planned using MRI images of the tumour and other methods. The radiation oncology doctor will decide on the length of the treatment and the radiation therapist works the machine that delivers the treatment.
Stereotactic radiosurgery: Single dose radiation
In radiosurgery, you get all of the radiation you need in a single day. It is given in a very focused form. The most common way of having radiosurgery is with a tool called a “gamma-knife”. The gamma-knife focuses more than 200 tiny beams of radiation onto the tumour with the aid of a stereotactic frame which is like a box fixed to the patient with four little screws placed with local anaesthetic.
Since the gamma knife can target very tiny spaces, the tumours come under control faster than the fractionated way and there may be less radiation to brain tissue near the tumour. But, the highly focused beams from the gamma-knife could mean that tiny areas around the tumour could also be harmed by the radiation, so it can only be used if it is safe to do so, based on the nearby structures. Gamma-knife radiosurgery is usually a one-time therapy completed in a single day although new techniques may allow a fractionated approach over a few days.
Side effects of radiation
All forms of radiation can damage normal pituitary and brain cells, which may lead to a loss of hormones over time. In rare cases, this damage may lead to memory loss or visual loss over several years. Radiation has a small risk of causing the growth of new tumours or cancers years after treatment.
Medicines
A third treatment option (to surgery and radiation) is medicine. Medicine can be used to:
- block the tumour from making too much hormone and sometimes reduce the size of certain types of pituitary tumours (prolactinomas and acromegaly)
- replace normal amounts of a hormone that has been lost due to pressure from the tumour or as a result of the effects of surgery or radiation.
Here are some medicines that patients with pituitary tumours might use. Ask your doctors and pharmacist for more information.
To treat prolactinoma
Cabergoline (or Dostinex®), Bromocriptine (or Parlodel®) and Quinagolide (Norprolac®) are three drugs that prevent the release of the prolactin hormone. They can be all that is needed to treat up to 90 per cent of all patients with prolactinomas.
Bromocriptine (or Parlodel®) and Quinagolide (Norprolac®) are taken once or twice a day whereas cabergoline (or Dostinex®) is usually given one to three times a week. All can have side effects, including nausea, dizziness and stuffy nose. These side effects happen less often with Cabergoline.
Cabergoline is more expensive but all three are generally covered by most drug insurance plans. Bromocriptine is covered for patients on Trillium or Ontario Drug Benefits (ODB).
To treat acromegaly
Octreotide (or Sandostatin®) reduces the release of growth hormone in acromegaly and sometimes reduces the tumour size modestly. It is given as an injection every three or four weeks by a nurse. Most commonly, it is used in addition to surgery. In rare cases, it may be used alone when surgery is not possible.
This drug can cause gallstones, abdominal cramps and diarrhea. It is very expensive and can be used before surgery or as a lifelong treatment. It is covered for patients on Trillium or Ontario Drug Benefits (ODB) and by most insurance companies.
Hormone replacement
As the master hormone gland, the pituitary produces 7 different hormones, which control other important hormone-producing glands. The hormones from these other glands may need to be replaced when levels are low:
Cortisol
Hydrocortisone (Cortef®) and prednisone are synthetic forms of the hormone cortisol. Either can be given to replace low amounts of the hormone in patients whose pituitary gland is not working properly. Too little hormone results in nausea, vomiting, dizziness, weakness and weight loss. Too much cortisol may cause symptoms similar to Cushing’s disease.
Thyroid hormone
Levo-thyroxine is the synthetic replacement for thyroid hormone. It comes in different strengths and preparations. It is taken with water first thing in the morning on an empty stomach. If you have low levels of thyroid hormone, you will feel tired, cold, constipated and may gain weight. Too much will make you feel anxious, with shaking hands and a racing heart beat.
Sex hormones
Pre-menopausal women who stop having periods due to a loss of pituitary function will need estrogen and progesterone to protect their bone density. These hormones are often given in the form of the birth control pills, or as patches.
Men will need testosterone therapy to restore sex drive and sexual function if this hormone level is too low. They will get this therapy as an injection in a muscle every two weeks, or as gels, patches or pills.
For fertility, both men and women will need other injected medicine, to replace the missing pituitary hormones (LH and FSH) if they have low levels of the pituitary hormones that control the function of the testes or ovaries.
Antidiuretic hormone (ADH)
ADH is a hormone that is made by the pituitary gland and causes the kidney to make concentrated urine. If the pituitary gland does not produce enough ADH, the body will make too much urine (over three litres a day) and the person becomes very thirsty.
DDAVP is a synthetic form of ADH. It is taken to increase the level of ADH in your body. DDAVP comes in different forms: as pills that are either melted under the tongue or swallowed, as a form that is sprayed into the nostril, or as an injection.
With more ADH in the body, the person will feel less thirsty and will not produce urine as frequently. The most common time for ADH to be low is right after surgery, but it usually comes back to normal levels after days to weeks.
Growth hormone
Finally, growth hormone levels can be low. This causes children to stop growing until they receive daily injections of growth hormone. Adults may feel very tired due to the lack of growth hormone, and may choose to take growth hormone therapy to improve their energy levels. Growth hormone therapy is very expensive, but the cost may be covered by private insurance or Trillium/Ontario Drug Benefits.
Many small tumours do not grow over time. These tumours can just be watched to see if they grow bigger. They may not need any active therapy. The growth of the tumour can be followed up by doing MRI scans about once every year. This plan can continue as long as the tumour is not causing symptoms (such as headaches or vision problems), is not growing, and is not affecting hormone production. This plan allows some patients to avoid surgery or radiation.
Please use this checklist to prepare for your first visit to the neurosurgeon or endocrinologist.
Two weeks before your first appointment
Make sure you have:
- Brought your MRI to your Neurosurgeon or Endocrinologist. If your MRI was not done at St. Michael’s Hospital, you will need to get the file from the film library of the Radiology Department at the hospital where you did your MRI.
- Completed all of your blood tests at St. Michael’s Hospital in the morning between 7:30 a.m. and 9 a.m.
- Completed your visual tests and the results were sent to your Neurosurgeon or Endocrinologist.
- Completed all special tests that were arranged for you.
- Made sure that notes from any other doctors and specialists were faxed to your neurosurgeon or endocrinologist.
- Know the names and addresses of all your doctors, including eye doctors.
- Made a list of all of your medicine and allergies.
- Made a list of all of your questions and thoroughly read this brochure/website content.
One week before your first appointment
The Endocrinology Clinic at St. Michael’s Hospital at 416-867-3679. If you do not speak English, please tell the office when you confirm your appointment. Interpreters are free for those who need them. Arrange to bring a family member or friend with you. Note: The office needs to book interpreters in advance.
On the day of your first appointment
Bring the following:
- All of your medicine and vitamins in their bottles.
- Health card or proof of other insurance.
- A family member or friend.
- Something to do in case you are waiting for a long time.
- A list of your questions.
- Bring your CD-ROM of your MRI.
Before you leave your first appointment, make sure you are clear about:
- Whether or not you are having surgery.
- Other tests that you need to do and who is arranging them.
- If you need any changes in your medicine.
- If you need any other appointments such as: ENT, Neuro-ophthalmology, CT scan, or radiation.
After your first appointment
If you are having surgery:
- You will get a phone call within one to two weeks of your appointment. We will tell you the date we propose for your surgery and any other testing or appointments.
- Read the information booklet or website content again.
- Stop smoking right away to prevent complications after your surgery.
- Undertake a regular exercise program to prepare for surgery and see your family doctor to make sure your general health is in order.
- Stop taking Aspirin or Clopidogrel (Plavix®) at least one week before surgery if this is okay with your family doctor. This will prevent abnormal bleeding during your surgery.
- Go to your appointment with the pre-admission facility.
If you are not having surgery:
Ask your Endocrinologist or referring family doctor about any questions you may have.
Preanesthesia Assessment and Testing Clinic
After you sign your consent forms, appointments will be made for you to attend the Preanesthesia Assessment and Testing Clinic (PATC). In the PATC, you will meet nurses who will prepare you for the day of surgery. The PATC appointment usually occurs days to weeks before the planned day of surgery. Make sure to bring all of your medicines, OHIP card, and inform staff of the names of your family members and referring doctors. Plan to spend at least half a day at the PATC. You will meet the nurse, the anesthesiologist and often the endocrinologist as well in PATC.
Surgery
You should confirm the time of surgery the day before the planned surgery date by calling the Sullivan Lounge (Tel: 416-864-5253) between 1 p.m. and 4:30 p.m. Please note: The Sullivan Lounge is closed on weekends and on statutory holidays. If your surgery is scheduled on a Monday or after a holiday, you must call on the Friday before your surgery.
You will need to arrive two hours before your scheduled surgery time to register: 6 a.m. is the earliest registration time. It makes sense to arrive very early – if the surgery before yours is cancelled, then your surgery can be done earlier than planned. If your surgery is scheduled for 7:45 a.m., it is very important to be there by 6 a.m.
Bring your valid Ontario Health Card and, if applicable, additional insurance coverage information.
What happens in hospital after surgery?
- Blood tests to check hormone levels or routine blood counts once or twice a day.
- Keeping track of how much is being drunk and how much pee (urine) is being produced is very important to make sure that the pituitary gland is making the right amount of the water hormone ADH. You will be asked to write down how much you are drinking. You will need to collect all your pee and give it to the nurse. The nurse will accurately measure how much urine you produce every day. If you get very thirsty and make too much urine, you may need to take a medicine called DDAVP (which acts like ADH). DDAVP will help your kidneys hold water in your body to prevent you from becoming dehydrated. Dehydration may cause low blood pressure.
- The same day or a day after surgery, the Vaseline gauze packing in the nostrils will be removed. It is common for some nose bleeding when it is removed but it usually stops within the first or second day. The nurses will show you how to gently wash your nose with salt water (saline) rinse once mild bleeding stops.
Checking for fever, blood pressure and pulse several times a day is routine.
How should I care for my nose after surgery?
It is important to take good care of your nose after surgery. You will need to rinse your nose six to eight times every day after you leave the hospital, for several weeks after the operation.
Do not blow your nose until the Ear Nose and Throat (ENT) surgeon has told you that your nose has fully healed. The pressure from blowing your nose can prevent the incision from healing and push germs up into the brain. If the incision opens out, brain fluid can leak out and germs can enter the brain to cause an infection called meningitis.
A stuffy nose or blocked feeling can last a few weeks. Gentle nasal washes with a sterile saline solution to clear out any blockages. For the first few weeks after surgery, use a gentle saline mist spray four to eight times per day. You can buy the spray at a local drugstore without a prescription.
Once the small plastic sheets in the nose are removed by the ENT Surgeon (usually two to three weeks after surgery), you can use a larger saline wash for your nose and sinus cavity. You can buy sterile saline packets and nasal rinse bottles at a local drugstore.
Instructions for nose saline washes
- Fill the nasal rinse bottle with 250mL (1 cup) of solution.
- While in the shower or over a sink, bend your head over and aim the head of the bottle nozzle away from the centre of your nose. Open your mouth and pour the saline solution in your nose. The fluid will circulate in and out of your sinus cavities, coming back out of your nose. It is okay if some of the solution comes out through your mouth. Try not to swallow large quantities.
- Repeat at least two to eight times a day (as a minimum, once in the morning and once in the evening), until the stuffiness is gone.
- After each use, rinse out the bottle and wash the tip with soap and water. Allow the bottle to air-dry completely. Once a week, sterilize the bottle by pouring 2/3 cup water and 1/3 cup of hydrogen peroxide into the irrigation bottle. Shake the solution and squirt it through the nozzle. Make sure the solution flows over the nozzle tip.
You can also make your own sterile saline solution by mixing 1 litre (1 quart) boiled or distilled water with 1 teaspoon canning/pickling/kosher salt (non-iodized) and 1 teaspoon baking soda.
If you make your own sterile saline solution, it is important to keep the solution in the refrigerator. Before using the solution, make sure it is at room temperature. You can warm up the solution by using a microwave. After using the microwave, make sure the solution is cooled to room temperature before using.
What should I be careful about after my surgery?
Sneezing: If you need to sneeze, keep your mouth open to avoid pressure.
Avoid straining yourself:
- while lifting
- during a bowel movement
- during sex
- do not blow your nose for three to four weeks after surgery and given the OK by the nose specialist or neurosurgeon
Straining increases pressure in your head and may damage the delicate surgical area. If the surgical area is damaged, this may cause a leak of cerebrospinal fluid.
Driving: Do not drive until you are off painkillers and your doctor says it is safe. Be sure to talk to your doctor before you drive. If your vision was affected before surgery, you will have to have a special visual field test and permission by the ophthalmologist before you are legally allowed to drive again. In many cases, the law requires that doctors report patients who might have impairments like loss of vision to the Ministry of Transportation and the Ministry may elect to suspend the patient’s driver’s license.
Travelling: Do not travel by airplane or go out of the country unless your doctor has checked your health and said it is safe. Do not plan to travel for at least 4 weeks after surgery and only once the surgeons and eye doctors say it safe to travel. Make sure to take along all of your medicine, as well as some of your medical notes describing your condition. Family doctors usually receive this information if you include your family doctor’s address and fax number when you register at the hospital.
Working: Most people are off work for about six to eight weeks, but some are off for more or less time.
Being active after your surgery
It is important to be active after surgery and to continue this at home. Gentle exercising will prevent complications after the surgery (such as pneumonia or a blood clot in your legs).
Walking often is the best exercise. Walk frequently and gradually for as long as you can every day. Try to walk for longer periods of time until you can walk for one hour without stopping. If you can’t walk for that long, try to do a little more each day.
Feeling tired is common and so short rests or even naps are OK.
Avoid heavy activities that may strain you.
Eating after your surgery
To prevent the result of straining (the need to strain during bowel movements):
- eat foods rich in fiber (such as whole grains, fruits such as prunes, leafy greens, and other vegetables),
- use stool softeners as needed (such as Colace).
Follow a normal balanced diet such as in Canada’s Food Guide.
What changes can I expect in my symptoms?
You will know that your surgery has been a success if you have the following changes in your symptoms.
If your vision was affected before surgery:
- some vision often returns within days or weeks of the surgery
If you have acromegaly or Cushing’s, your treatment is a success if:
- your hormone levels return to normal
- some of the changes that the tumour has caused go away
If you have a prolactinomas, your treatment is a success if:
- your menstrual periods return
- your fertility improves
- milk production stops
- you have improved sexual function or desire
If you have a large tumour and get headaches because of the tumour, your headaches will have a good chance of improving.
Follow-up appointments
After surgery, the staff in the hospital will arrange appointments for you to see:
- ENT surgeon in two to three weeks
- Endocrinologist in two to four weeks
- Ophthalmologist or optometrist for visual field testing and OCT in four weeks
- MRI in four weeks
- Neurosurgeon in six to eight weeks (along with an MRI of the pituitary gland before you see your neurosurgeon)
- Family doctor every week for the next few weeks after your surgery
When should I contact my doctor or nurse?
Call 911 immediately or have someone take you to the nearest emergency hospital if you notice any of the following:
- Significant bleeding that does not stop with pressure or if there is a sudden gush of blood from your nose.
- Severe pain
- Fever (above 38.5°C or 100.5°F)
- Worsening headache
- Stiff or sore neck especially if fever is present
- You feel very weak, nausea (dizzy) or are vomiting
- Confusion
- Worsening vision
Call your neurosurgeon or nurse practitioner if you notice any of the following:
- Worsening pain
- Stiff neck or headache
- Vision is worse
Call your ENT surgeon if you notice:
- Nasal discharge or bad smell
- Nose bleeding
- Clear or yellow nasal fluid leakage
Call your endocrinologist if you:
- Are very thirsty or if you produce a lot of urine (pee)
- Extreme weakness
If in doubt, please contact a health professional.
Most patients respond well to treatment and have non-cancerous tumours. For long-term follow-up most patients will need a yearly MRI of the pituitary gland and yearly visual fields eye tests, and regular visits with the endocrinologist and ophthalmologist or optometrist.
Family doctors need to make sure that patients get these tests and appointments on a regular basis so it is essential that patients regularly see their family doctor to arrange the tests. If patients have any new surgical issues, the family doctor should refer you back to the neurosurgeon.
Health Connect Ontario (to call or chat online with a registered nurse): https://healthconnectontario.health.gov.on.ca/
Canada’s Food Guide: https://food-guide.canada.ca/en/
Distress Centres of Toronto (If you are feeling distressed and need to talk)
416-408-HELP (4357)
Members of the team and how to contact us
| Neurosurgeons | |
|---|---|
| Dr. Michael Cusimano | Tel: 416-864-6048; Fax: 416-864-5857 |
| Dr. Saira Alli | Tel: 416-360-4000 x78191; Fax: 416-864-3016 |
| Endocrinologists | |
| Dr. Jeannette Goguen | Tel : 416-867-3714; Fax: 416-867-3724 |
| Dr. Gillian Booth | Tel: 416-867-3719; Fax: 416-867-3724 |
| Neuro-Ophthalmologist | |
| Dr. Irene Vanek | Tel: 416-864-5945; Fax: 416-864-5953 |
| Otolaryngologists (ENT) | |
| Dr. John Lee | Tel: 416-864-5306; Fax: 416-864-5469 |
| Dr. Jennifer Anderson | Tel: 416-864-5278; Fax: 416-864-5367 |
| Dr. Yvonne Chan | Tel: 416-864-5279; Fax: 416-864-5694 |
| Social Worker | |
| Rebecca Blidner | Tel : 416-864-6060 x2125 |
| Nurse Practitioners (neurosurgery) | |
| Tom Willis | Tel: 416-864-5039 |
| Theresa Cook | Tel: 416-360-4000 x2980 |
| Martine Andrews | Tel: 416-864-6060 x2951; Fax: 416-864-5790 |
| Jenny Pak | Tel: 416-864-6060 x3409 |
| Elyse Kalpage | Tel: 416-864-6060 x6978 |
| Clinics | |
| Neurosurgery Clinic | 3 Donnelly Wing South Tel : 416-864-5678; Fax: 416-864-5790 |
| Endocrinology Offices | 6th Floor/61 Queen Street East |
| Endocrinology Clinic | 7th Floor/61 Queen Street East Tel : 416-867-3679 |
| ENT Clinic | 8 Cardinal Carter North Tel: 416-864-5276; Fax: 416-864-5694 |
| MRI | B2 Cardinal Carter South Tel: 416-864-5661; Fax: 416-864-5820 |
| Pre-Admission Facility (PAF) | 10 Donnelly Tel : 416-864-5689 / 416-864-6074 / 416-864-5436; Fax: 416-864-5199 |
| Information about blood transfusion | |
| Blood Transfusion Service | Tel: 416-864-5084 |
| Transfusion Coordinator | Tel: 416-864-6060 x4055 |
Terms of use agreement
It is important that you read all the following terms and conditions carefully. This Terms of Use Agreement (“agreement”) is a legal agreement between you and The Interdisciplinary Pituitary Disorders Centre of Excellence, the owner and operator (“owner”) of this website (the “website”). It states the terms and conditions under which you may access and use the website and all written and other materials displayed or made available through the website, including, without limitation, articles, text, photographs, images, illustrations, audio clips, video clips, computer software, and code (the “content”). By accessing and using the website, you are indicating your acceptance to be bound by the terms and conditions of this agreement. If you do not accept these terms and conditions, you must not access or use the website. The owner may revise this agreement at any time by updating this posting. Use of the website after such changes are posted will signify your acceptance of these revised terms. You should visit this page periodically to review this agreement.
Medical Emergency
Do not use the website for medical emergencies. If you have a medical emergency, call a physician or qualified healthcare provider, or call 911 immediately. Under no circumstances should you attempt self-treatment based on anything you have seen or read on the website.
General information is not medical advice
The general information provided on the website is for informational purposes only and is not professional medical advice, diagnosis, treatment, or care, nor is it intended to be a substitute therefore. Always seek the advice of your physician or other qualified health provider properly licensed to practise medicine or general health care in your jurisdiction concerning any questions you may have regarding any information obtained from this website and any medical condition you believe may be relevant to you or to someone else. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. Always consult with your physician or other qualified healthcare provider before embarking on a new treatment, diet, or fitness program. Information obtained on the website is not exhaustive and does not cover all diseases, ailments, physical conditions, or their treatment.
No endorsements
Unless specifically stated, the owner does not recommend or endorse any specific brand of products, services, procedures, or other information that appears or that may be advertised on the website.
Communications
Communications sent by you to the owner or your physician, or to you by the owner or your physician via email or this website may not be secure and may be accessible by third parties. Any use or disclosure of personal information provided by you shall be in accordance with our privacy policy.
The owner does not wish to use this website as a means of communication with the public (i) regarding questions or issues of a medical nature; (ii) to establish physician-patient relationships; (iii) to book or cancel appointments; or (iv) for inquiries regarding fees, services, or similar matters. Email communications regarding such matters will not be responded to and will be discarded unread.
Disclaimer of warranties
The website and the content are provided “as is” and “as avialable.” While the owner endeavours to provide information that is correct, accurate, current, and timely, the owner makes no representations, warranties, or covenants, express or implied, regarding the website and the content including, without limitation, no representation, warranty, or covenant that (i) the content contained in or made available through the website or any item(s) made available on or through the website will be of merchantable quality and/or fit for a particular purpose; (ii) the website or content will be accurate, complete, current, reliable, timely, or suitable for any particular purpose; (iii) that the operation of the website will be uninterrupted or error-free; (iv) that defects or errors in the website or the Content, be it human or computer errors, will be corrected; (v) that the website will be free from viruses or harmful components; and (vi) that communications to or from the website will be secure and/or not intercepted.
You acknowledge and agree that your access and use of the website and the content is entirely at your own risk and liability.
Copyright
The content is protected by copyright law and is owned by the owner and its licensors, or the party accredited as the provider of the content. Except as granted in the limited licence herein, any use of the content, including modification, transmission, presentation, distribution, republication, or other exploitation of the website or of its content, whether in whole or in part, is prohibited without the express prior written consent of the owner.
Limited Licence
Subject to the terms and conditions of this Agreement, you are hereby granted a limited, nontransferable, and non-exclusive licence to access, view, and use the website and the content for your personal, non-commercial use. You are granted the right to download, store, and/or print single copies of items comprising the content for your personal, non-commercial use, provided that you maintain all copyright and other notices contained in such content. You may not copy and/or repost items comprising the content online. You must also abide by any additional requirements governing the use of any specific content that may be set out in the website. In the event of a conflict between the terms of a licence governing specific content and this agreement, the terms of the specific licence shall govern.
Termination
The owner may, in its sole discretion, cancel or terminate your right to use the website, or any part of the website, at any time without notice. In the event of termination, you are no longer authorized to access the website, or the part of the website affected by such cancellation or termination. The restrictions imposed on you with respect to material downloaded from the website and the disclaimers and limitations of liabilities set forth in this agreement, shall survive termination of this agreement. The owner shall not be liable to any party for such termination.
Last updated August 29, 2024







