Our Education Team

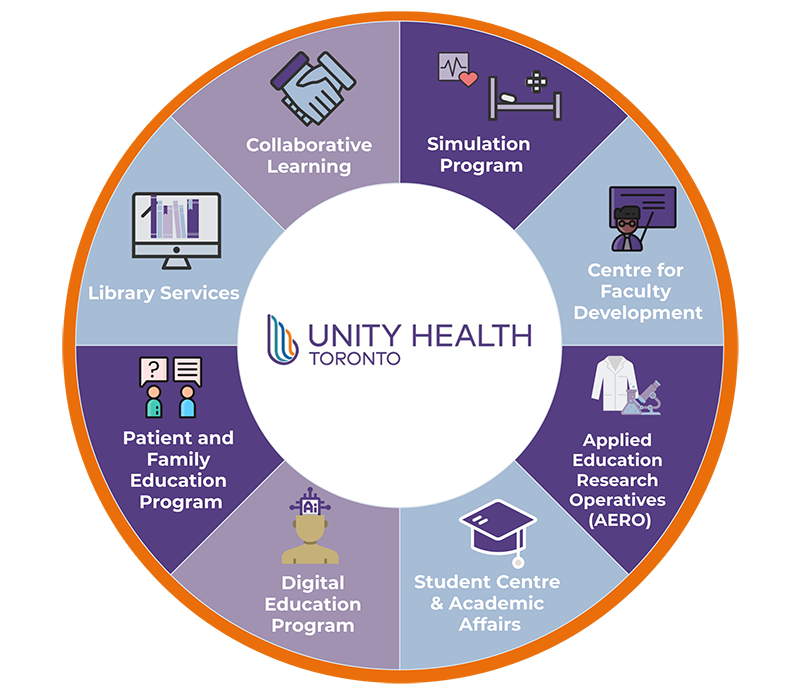
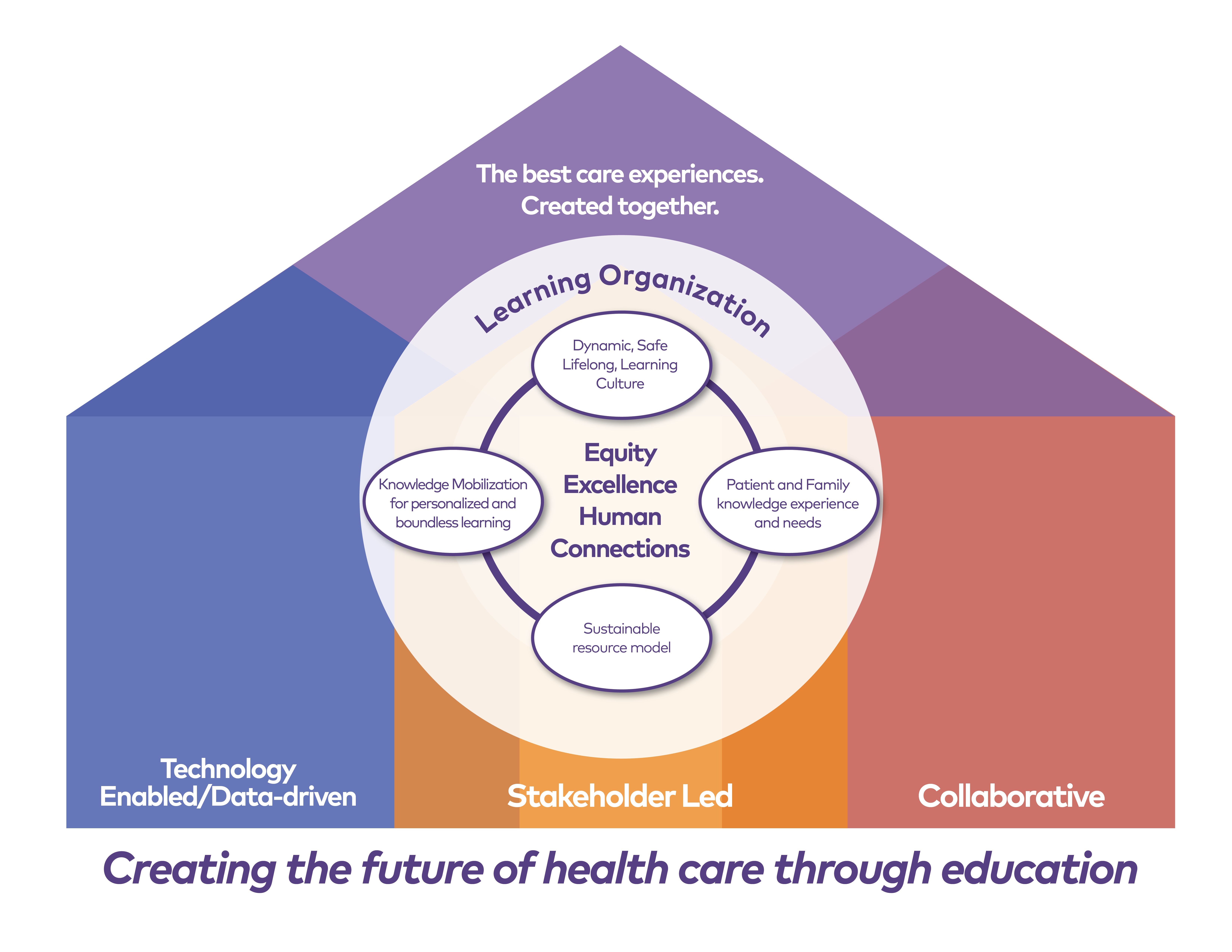
In 2019, Unity Health Toronto committed to devote the next five years to reimagining teaching and learning across the organization. The Education Portfolio puts human connection at the centre of all of our decisions so that we can deliver excellent education with our academic partners while supporting the wellness and safety of our learners and educators.
The best care experiences created together.
Reimagining teaching and learning.
We are excited to embark on a new education strategy for Unity Health Toronto with a commitment to practice a data-driven, stakeholder-led and collaborative approach to achieving our strategic priorities.

Sasha Miles is our Director of Clinical & Integrated Education. This department supports all of Unity Health Toronto’s incoming and existing learners across all three sites.
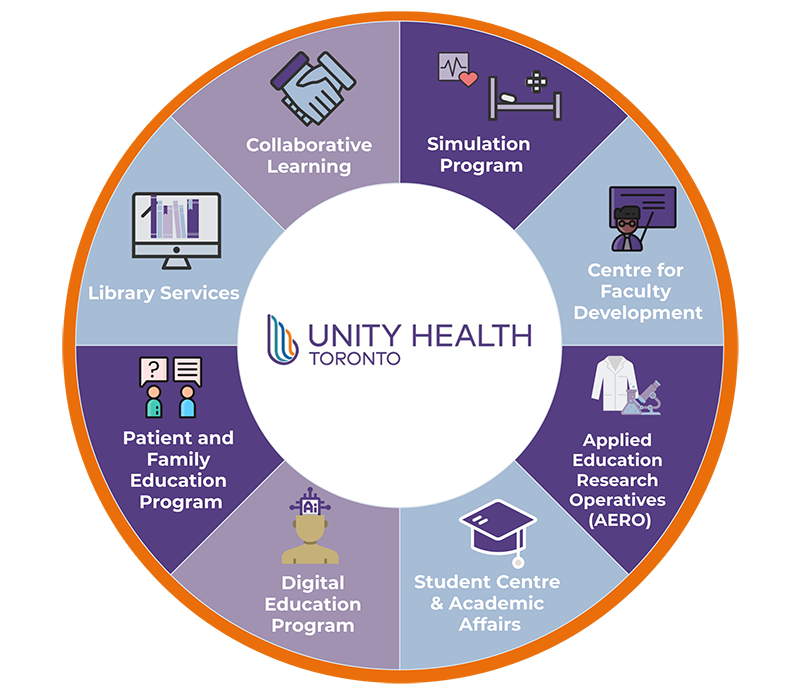
Collaborative Education Program >>Collaborative Learning (CL), also known as Interprofessional Education (IPE), provides staff and learners with experiences to learn about, from, and with each other. Our Collaborative Learning Program provides faculty development opportunities for Unity Health staff and physicians such as Teaching for Learning and Collaboration (TLC) and Collaborative Learning Facilitator training. Through partnership with the University of Toronto’s Centre for Interprofessional Education, we are also able to offer a variety of accredited interprofessional opportunities for learners, including our CL student series, structured placements, and peer mentorship. For more information please contact Collaborative.Learning@unityhealth.to.
Our Student Centre supports a superior student experience for all students at Unity Health Toronto through the provision of a centralized administrative and support hub for all student activity. The Student Centre is a welcoming environment that supports over 6,000 students annually from all student types, including Health Disciplines, Nursing, Medicine (undergraduate and postgraduate), Administrative, and Operational. Any student completing a placement at Unity Health Toronto must be registered with the Student Centre prior to starting their placement. For more information please contact:
The University of Toronto MD Program delivers portions of the curriculum via the academy structure. St. Michael’s and St. Joseph’s are the anchor sites for the FitzGerald Academy. At our Academy, our students learn clinical skills, participate in case-based learning, and have opportunities to participate in interprofessional educational activities. Our clinicians are dedicated to excellence in medical education and provide medical students with the hospital-based portions of the curriculum. We bring together amazing students and dedicated, compassionate teachers in a setting that is focused on providing the best clinical care to our patients. For more information please visit FitzGerald Academy | MD Program.
Unity Health Toronto collaborates with our academic and community partners to offer a wide variety of clinical, non-clinical, and research learning opportunities for students requiring experiential placements as part of an academic course. We aim to provide support and resources to ensure that student learning experiences are collaborative, innovative, diverse, and positive. We support and enhance the student experience through collaboration with our staff, students and patients & caregivers. Student placements at our sites must be supported by an Academic Affiliation Agreement between the School and Unity Health Toronto. For more information please contact academicaffairs@unityhealth.to.
The Patient and Family Education Program is available across Unity Health Toronto. Our program works with staff, physicians, and learners to create patient education resources, enhance communication materials, and help patients and families navigate their health care journey. For more information about our program please contact patienteducation@unityhealth.to.
The Patient and Family Learning Centres help visitors learn more about health conditions and applicable community services that may be available. We are open to all patients, families, caregivers, community members and staff. Our teams will work with you to answer your questions and guide you to easy-to-understand resources that meet your needs. To access our online repository of health resources visit our Online Health Library. Our physical Learning Centres are located at:

Nazanin Khodadoust is our Director of Technology Enabled Education. This department strives to mobilize knowledge and technology to provide the best education experience for everyone at Unity Health Toronto.
Digital & Virtual Education Program >>The Digital Education arm supports the design and development of online learning initiatives across Unity Health Toronto. As an educator within Unity Health Toronto, whether you want to create an interactive e-learning course, develop an online quiz, or coordinate enrolment for synchronous education sessions, our team of educational technology and adult learning experts can help you bring your digital education projects to fruition. For more information, please contact learning@smh.ca.
The Virtual Education arm at Unity Health Toronto collaborates with teams to help design and implement virtual learning experiences. From pedagogical considerations, best practice guidelines and policies, workflow design, and platform and equipment selection, the Virtual Education team helps our educators deliver their learning objectives remotely to a broad audience anywhere in the world. For more information, please contact virtualeducation@unityhealth.to.
During the COVID-19 pandemic, the Virtual Education team developed and championed best practices around virtual supervision so that our learners could feel confident and continue practicing in any environment. If you are a Unity Health Toronto learner providing virtual care, virtual supervision may be an option to discuss with your supervisor.
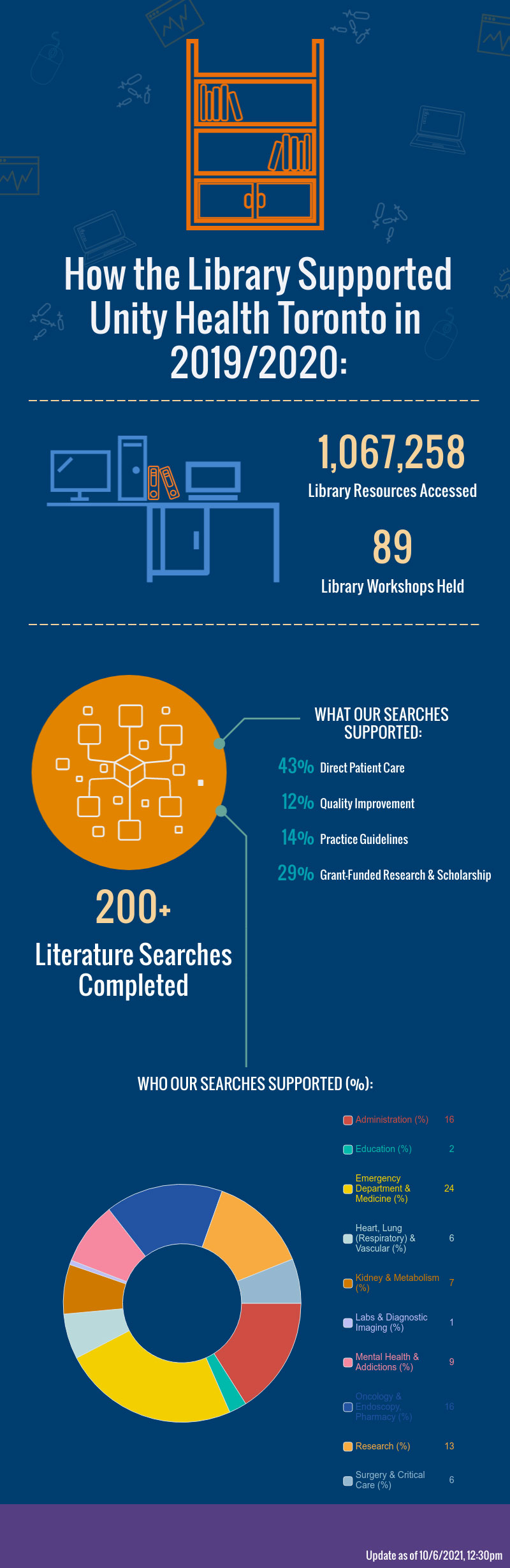
• Library Services supports education, research, and evidence-based decision-making for all physicians, staff, and learners at Unity Health Toronto. Students and residents have unlimited access to library electronic resources (databases, e-journals, e-books, software, clinical decision support tools), borrowing privileges for print collections, interlibrary loan services, dozens of library workshops and custom training opportunities. We also provide 24/7 access to library spaces for independent study, computer-use, and printing, scanning, photocopying. Information Specialists are available to support all learning, research, and information needs. For more information please contact:
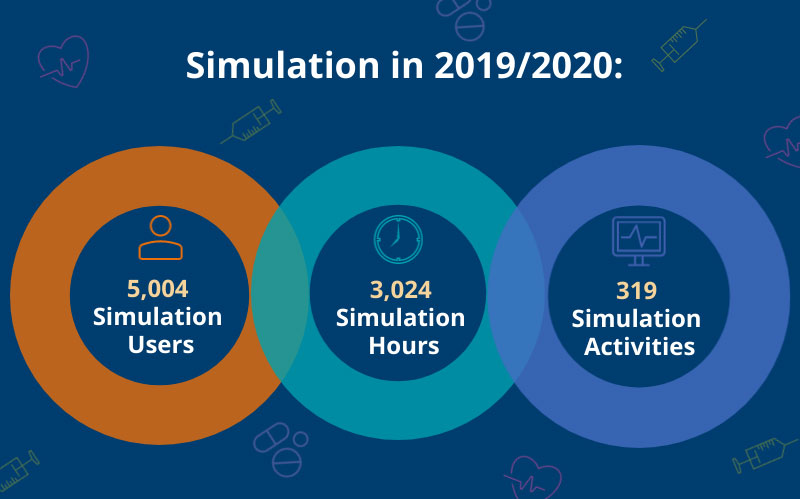
Unity Health Toronto’s state of the art Simulation Program allows students, health disciplines and nursing professionals, researchers, administrators and physicians to practice skills in a safe, realistic learning environment using high fidelity human patient simulators, virtual reality, and task trainers. Health care simulation involves a range of activities that share a similar purpose: to improve patient safety and quality of care, provide interprofessional education opportunities, and increase the effectiveness and efficiency of health care services. The Royal College of Physicians and Surgeons of Canada currently accredits (2019-2024) the Allan Waters Family Simulation Program at St. Michael’s Hospital. This national accreditation recognizes leaders in simulation-based learning and educational research. Our goal is to obtain of obtaining Royal College accreditation at all of our sites. For more information please contact simulationprogram@unityhealth.to.

Latika Nirula is our Director of the Centre for Faculty Development (CFD). The department offers programming focused on system needs and integrating faculty development and education research into practice.
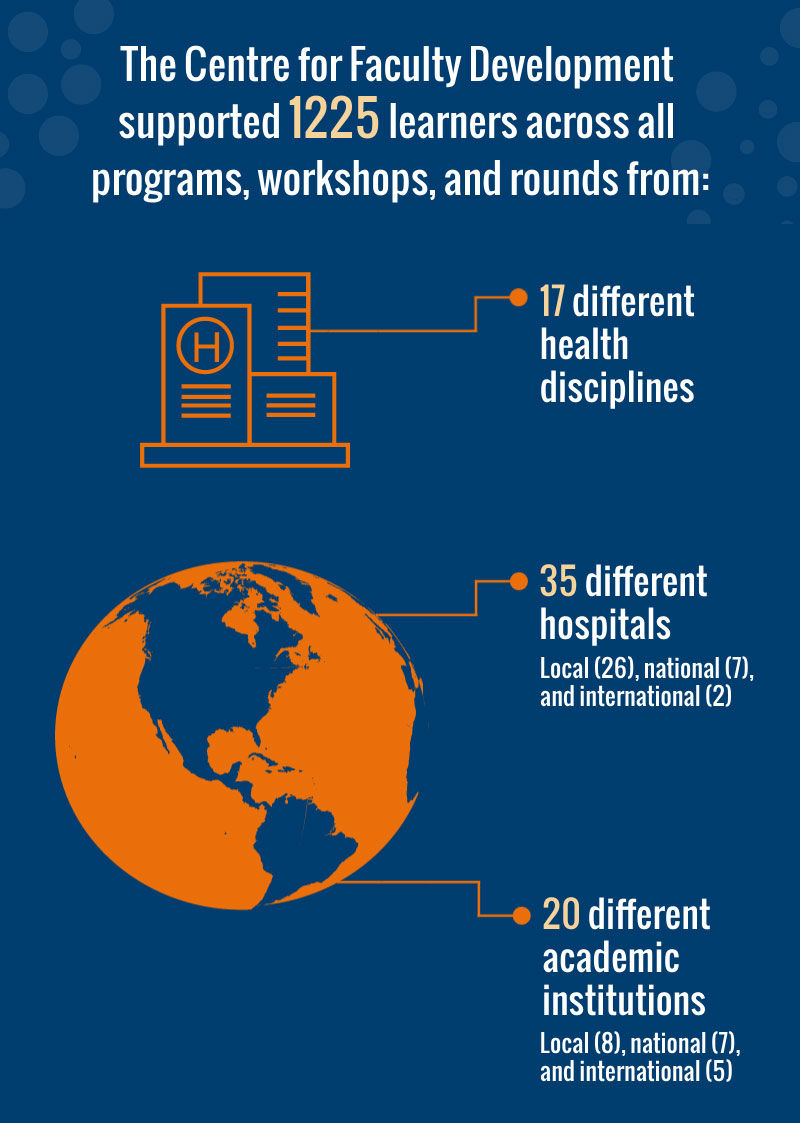
Department details >>The Centre for Faculty Development (CFD) was founded in 2002 as a partnership between St. Michael's Hospital (now known as Unity Health Toronto) and the University of Toronto, Temerty Faculty of Medicine. At the CFD we are committed to supporting health professionals in their multiple education roles and activities – including teaching, academic leadership, scholarship and advocacy. We offer flexible and adaptable programming that is responsive to emerging needs, facilitates communities and networking, and supports capacity building across the system. The CFD offers faculty development consultations with local, national and international partners. For more information, please visit cfd.utoronto.ca.

Ryan Brydges holds the Professorship in Technology-Enabled Education and serves as the Director of the Applied Education Research Operatives (AERO) Research Platform. AERO bridges education research, health professions teaching, and healthcare practice to advance top-quality, compassionate care experiences.
Department details >>The Applied Education Research Operatives (AERO) is a group of educators/scholars from across Unity Health Toronto, who share a common commitment to doing impactful work by bridging education science and innovative education. AERO partners with many individuals, organizations, and units locally, nationally, and internationally. Our closest partners are the Allan Waters Family Simulation Centre and the Centre for Faculty Development. For more information please visit www.aerotoronto.ca.
AERO serves two main groups:


Stakeholder Led
We strive to support initiatives led by impacted stakeholders whenever possible, whether that be staff, students, or faculty.

Collaborative
We believe that the best work doesn’t occur in siloes, so we strive to foster environments for interdisciplinary collaboration.

Data-driven
We want to ensure that we are accountable for our promises and are able to be proactive in our decisions, being data-driven will allow us to spot opportunities and gage impact.
We have had another excellent year in teaching and learning at Unity Health Toronto. I am grateful to be a part of such an exceptional and committed network of professionals dedicated to creating supportive learning environments and programs for learners, staff and physicians across all health disciplines, as well as advancing knowledge and skills to enable safe and effective care for our patients, residents and their families.
At Unity Health Toronto we want to shift our teaching and learning paradigms from reproducing the world to transforming it. Our ultimate goal is to create the most effective and compassionate care experience and our focus is ensuring our teaching and learning environments will get us there.
This year was about evolution for the Education portfolio as we worked to establish a leadership structure to meet the needs of Unity Health’s corporate and education strategic plans and ensured equitable support across our three sites. We focused on a goal to support equitable access to education, evaluate programming and provide evidence-based education for the network. We also prioritized improvements to our learning environment and worked to highlight the structures and processes available to support the experience our learners have. Our work in these areas was recognized in feedback we received through our learner survey and I’m proud to share some examples that reflect the efforts of the Education team:
“I have learned that Unity Health Toronto is a great foundation. In speaking with my unit manager, I realized how fully committed to diversity and inclusion this hospital is. Also, the resources available to students is second-to-none. I have never been treated like I mattered or had a right to attend my clinical placement as much as I did when working at Unity Health.”
I also want to acknowledge the unprecedented changes and challenges we faced this year because of the global COVID-19 pandemic, which required our portfolio to be creative and flexible when we needed to pause our in-person student programming. The safety of our learners is our top priority and we recognized the need to shift our education to a virtual platform.

Despite the obstacles we faced with the COVID-19 pandemic, the Education portfolio accomplished a great deal of important work in 2019-20. There are many highlights to share and it is my pleasure to celebrate the successes we have achieved together this year in our Annual Report. Enjoy!
Sincerely,
Beverly Bulmer, Vice-President of Education, Unity Health Toronto
We will embody a dynamic, safe, lifelong teaching and learning culture that drives excellence, equity, and values human connections.
Ensuring that our learners are safe and have an excellent experience at Unity Health is vital to us; that’s why harmonizing the Student Registration System (SRS) was such a huge accomplishment. With the generous support of the Providence Foundation we were able to partner with Unity Health Toronto’s IT and the IT PMO teams to build the SRS in-house.
This year we transformed the Stepping Stones curriculum based on the needs in the system and the gaps that faculty have identified. We shifted our curriculum to a cohort-based delivery model which offers increased opportunities for networking and collaboration between an interdisciplinary group of faculty members The design of the new curriculum ensures that we can be agile to meet the constantly evolving needs of our educators.

Stakeholder Led
Content for the event was curated based on issues voiced by staff members with lived experiences and local EDI experts to help Unity Health Toronto faculty create safer and more inclusive learning environments.

Collaborative
FDD is a collaboration between the Centre for Faculty Development (CFD) and the Education at Unity Health Toronto. Community panelists led workshops focused on EDI topics such as creating culturally safe practices through storytelling, employing reflexive learning, identifying barriers to accessibility to help attendees get familiar with leaning into discomfort.

Data-driven
Due to the incredible interest generated by the topic, we filled our in-person seats in a matter of a few days and broadcasted the keynote presentation via Zoom to make the event accessible to a broader audience. The feedback collected through the post-event evaluation will be used to inform future event offerings.
We will embed patient, resident, and family voices, knowledge, and learning needs into everything we do.


Stakeholder Led
PEEP was commissioned to embed patient, caregiver, and resident voices into teaching and learning at Unity Health Toronto. We co-created the terms of reference with patient/family partners at the table.

Collaborative
This committee solidified the collaboration between the Patient and Family Education team and the Patient Experience and Community team at Unity Health Toronto. Together with our Patient and Family Partners we identified two key committee priorities: creating an organizational health literacy index and a patients and family as educators curriculum.

Data-driven
Videoconferencing allowed us to maximize committee participation across staff at all three sites and off-site with our Patient and Family Partners.

Stakeholder Led
This workshop was developed to set the standard for best practices in involving patient voices in health professions education. Patients were involved in informing the creation of the curriculum and co-facilitating.

Collaborative
With facilitated guidance, participants have the space to reflect and articulate the ethical and social complexities of their practices. The workshop was co-developed and co-facilitated by Sacha Agrawal from CAMH, Paula Rowland from the Wilson Centre, and Rachel Wilson, a service user educator.

Data-driven
The curriculum was underpinned and informed by both lived experiences and the practice-based and research knowledge of our facilitators; the central framework shared in the workshop is based on the empirical work led by Paula Rowland from the Wilson Centre.
We will mobilize knowledge, data and technology to create the most relevant, personalized, accessible learning for all.

As part of our goal to create an organization-wide simulation program we secured a partnership with the Providence Healthcare Foundation for the development of simulation program capacity at Providence. Our team of simulation experts consulted with a wide variety of professional practice leaders and clinicians from Providence to inform the design of the space in a way that met the institution’s specific needs.

Stakeholder Led
Key stakeholders in our labour and delivery unit saw an opportunity for quality improvement when it came to completing transfers and consults to their department safely and respectfully. The project was led by an interdisciplinary team of stakeholders (e.g. OB, Midwifery, Nursing, Quality and Safety, Knowledge Mobilization Researchers, Simulation Program).

Collaborative
Bringing together this diverse array of stakeholders to address a shared challenge allowed us to merge practical knowledge, education science, and simulation to improve care quality and experience for mothers and their babies.

Data-driven
Ethnographic methods and the implementation of tabletop and in-situ simulations helped the team dissect the complex issue to develop and trial policy changes. Tangible and immediate policy changes were made based on this study locally and internationally. Multiple peer-reviewed publications are currently in review.
We will have a sustainable and responsive resource model that enables strategic investments in teaching, learning and education research.

The St. Joseph’s Learning Centre provides a dedicated space for learning and professional development activity. The project was funded by the St. Joseph’s Health Centre Foundation. It was designed based on robust consultations with student centre staff, professional practice and clinical preceptors.

Stakeholder Led
Unity Health Toronto had three separate learning management systems which led to redundancies for learners and staff who had to complete and manage modules across multiple sites. We conducted a needs assessment to understand the unique requirements of each site.

Collaborative
Our eLearning team worked with IT and HR to design and build a harmonized eLearning Management System that provides equal opportunities and standardizes the experience for all Unity Health Toronto learners and staff, and supports cross-site initiatives (e.g. orientation).

Data-driven
Our single system provides a platform to standardize learning, performance appraisal and professional development opportunities. It allows us to track completion data and work towards building a personalized approach to mandatory and preferred learning and development.



As of March 2020, our in-person student programming came to a halt due to COVID-19. Managing the effects of the pandemic on learngers required our portfolio to be creative, nimble and flexible. Where possible, we shifted education to a virtual platform online. As our fiscal year came to a close we continued to work with our post-secondary academic partners and fellow academic health-care institutions to monitor the situation and ensure that our learners' safety was of the utmost priority.
Fresh off the successful simulations that supported the opening of the new St. Michael's Trauma Bay, our Simulation Program quickly pulled together a team and used rapid cycle simulations over two days to support the opening of the St. Michael's COVID-19 Assessment Centre (CAC). Starting with a tape and cardboard mockup of the proposed space, the Simulations Program took our colleagues through simulations that became more and more realistic over time which allowed us to gather nuanced user perspectives and identify any points of confusion in the process. This occured in tandem with the CAC physically being built.
During the peak of the COVID-19 pandemic, CFD and AERO partnered with organizations and researchers from across the University of Toronto and the Toronto Academic Health Sciences Network (TAHSN) to develop the Quick ICU Training Resource.
The goal of this resource was to provide quick, accessible learning resources and reference materials for clinicians who are upskilling, renewing or reviewing their knowledge and skill for the redeployment to critical care due to the demands of the pandemic.
The 2020-2021 fiscal year has largely been devoted to adapting to the new normal. The Education Portfolio has spent a majority of our time and resources discovering how to best support our students, staff, and physicians as they continue to navigate learning, teaching, and providing care during the COVID-19 pandemic. This section highlights the diverse array of projects and initiatives our teams have led this year.
We are all students here at Unity Health Toronto and value any opportunity to receive feedback.
Please share your feedback, questions, or ideas with us!
30 Bond Street, Toronto, Ontario, M5B 1W8, Canada
416-360-4000